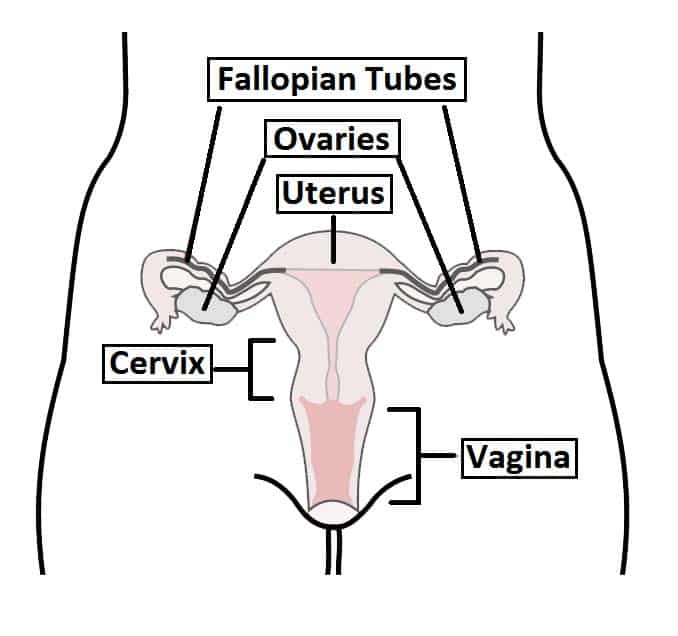
The cervix is the lower portion of the uterus, forming the narrow canal that connects the vagina with the uterine cavity. Functioning as a gateway between the external and internal reproductive tracts, the cervix plays a vital role in reproductive health.
Although continuous with the uterus, the cervix is anatomically and histologically distinct and is therefore considered as a separate structure.
In this article, we will look at the anatomy of the cervix – its structure, neurovascular supply and clinical correlations.
Pro Feature - 3D Model
Anatomical Structure
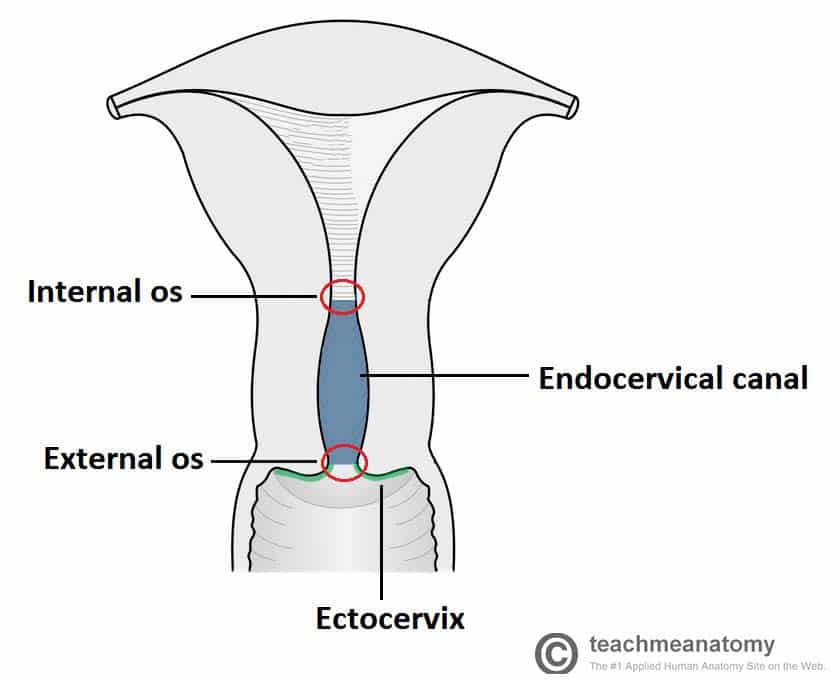
The cervix is comprised of two main regions—ectocervix and endocervical canal—and contains two openings: the external os and the internal os.
- Ectocervix – the portion that projects into the vaginal lumen. It is lined by non-keratinised stratified squamous epithelium. The central opening, called the external os, leads into the endocervical canal.
- Endocervix (endocervical canal) – the inner canal that extends from the external os to the internal os, where it opens into the uterine cavity. It is lined by mucus-secreting simple columnar epithelium.
Pro Feature - Dissection Images


Functions
The cervix serves two main functions:
- Sperm entry – permits the entry of sperm into the uterus, particularly during ovulation when cervical mucus becomes thinner and more receptive.
- Barrier function – forms a physical and immunological barrier that helps maintain sterility in the uterus. This is achieved through tight cervical closure, thick mucus, and periodic shedding of the endometrial lining.
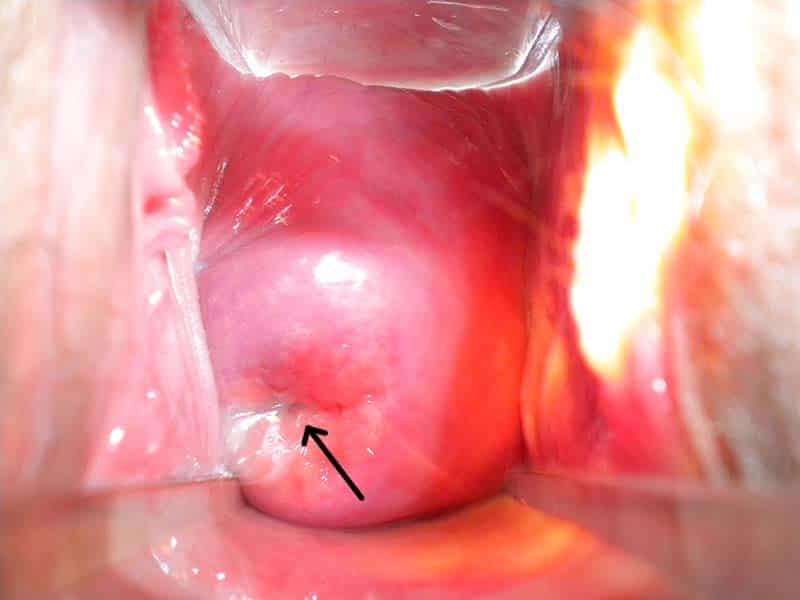
Fig 3
The ectocervix, visible via a speculum inserted into the vagina. The external os is marked with an arrow.
Neurovascular Supply
The cervix receives its arterial supply primarily from the uterine artery, a branch of the internal iliac artery. Venous drainage is via the uterine venous plexus, which drains into the uterine veins and then into the internal iliac veins.
Innervation is provided by the uterovaginal plexus, a branch of the inferior hypogastric plexus. Sympathetic fibres (T10–L2) are responsible for pain sensation, particularly during menstruation or labour. Parasympathetic fibres (S2–S4), via the pelvic splanchnic nerves, contribute to motor and secretory functions.
The cervix has limited somatic sensory innervation, which explains why some procedures (e.g. cervical smear or IUD insertion) may be well tolerated without anaesthesia.
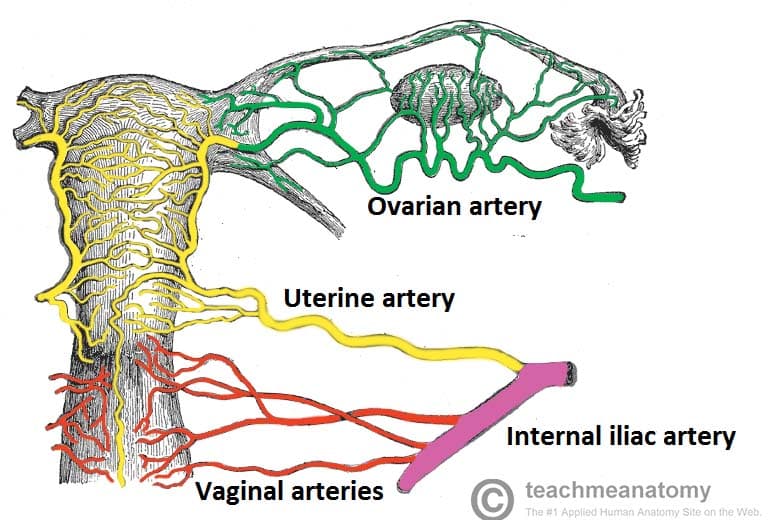
Fig 4
Posterior view of the arterial supply to the female reproductive tract.
Lymphatic Drainage
Lymph from the cervix drains to the iliac, sacral, aortic, and inguinal lymph nodes.
Clinical Relevance
Cervical Insufficiency
Cervical insufficiency (also known as cervical incompetence) occurs when the cervix is unable to remain closed during pregnancy, leading to premature dilation and potential pregnancy loss.
This condition highlights the mechanical barrier role of the cervix, particularly the internal os.
Management options include cervical cerclage – where a sugical suture is placed around the cervical to maintain its closed state.