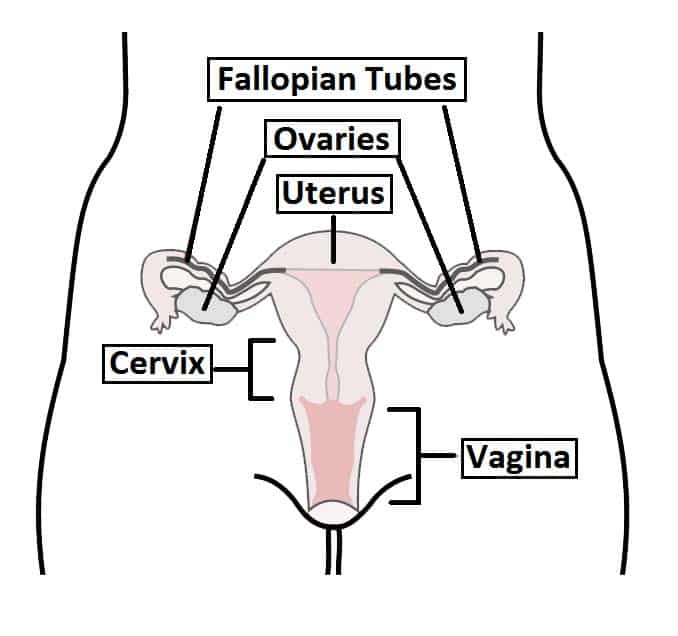
The vagina is an organ of the female reproductive tract. It is a distensible muscular tube which extends posterosuperiorly from the external vaginal orifice to the cervix.
It has several roles within the female reproductive system:
- Sexual intercourse – receives the penis and ejaculate, assisting in its transport to the uterus.
- Childbirth – expands to provide a channel for delivery of a newborn from the uterus.
- Menstruation – serves as a canal for menstrual fluid and tissue to leave the body.
In this article, we will look at the anatomy of the vagina – its structure, innervation, vascular and lymphatic supply.
Anatomical Position
The vagina is closely related to many of the organs in the pelvic region:
- Anterior – bladder and urethra.
- Posterior – rectouterine pouch, rectum and anal canal.
- Lateral – ureters and levator ani muscle.
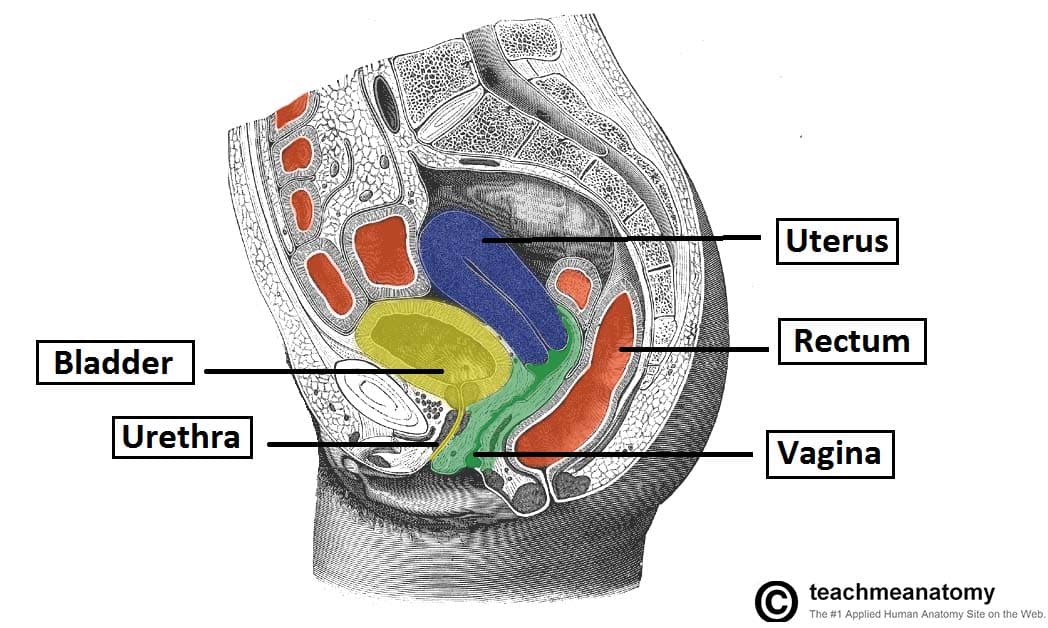
Fig 2 – Sagittal section of the female pelvis, showing the anatomical relations of the vagina.
Anatomical Structure
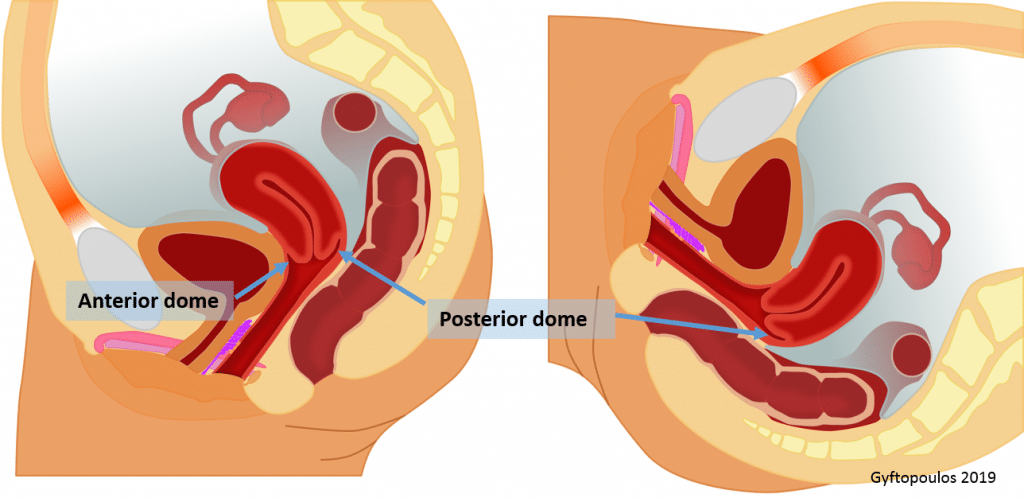
The vagina is a fibromuscular tube with anterior and posterior walls – these are normally collapsed and thus in contact with one another.
The shape of the vagina is not a round tunnel. In the transverse plane it is more like an “H” lying on the side. At the upper ending, the vagina surrounds the cervix, creating two domes (fornices or vaults): an anterior and a (deeper) posterior one.
The posterior fornix is important as it acts like a natural reservoir for semen after intravaginal ejaculation. The semen retained in the fornix liquefies in the next 20-30 mins, allowing for easier permeation through the cervical canal.
Histology of the Vagina
The vagina is composed of four histological layers (internal to external):
- Stratified squamous epithelium – this layer provides protection and is lubricated by cervical mucus (the vagina itself does not contain any glands).
- Elastic lamina propria – a dense connective tissue layer which projects papillae into the overlying epithelium. The larger veins are located here.
- Fibromuscular layer – comprising two layers of smooth muscle; an inner circular and an outer longitudinal layer.
- Adventitia – a fibrous layer, which provides additional strength to the vagina whilst also binding it to surrounding structures.
Vascular Supply and Lymphatics
The arterial supply to the vagina is via the uterine and vaginal arteries – both branches of the internal iliac artery.
Venous return is by the vaginal venous plexus, which drains into the internal iliac veins via the uterine vein.
Lymphatic drainage is divided into three sections:
- Superior – drains to external iliac nodes
- Middle – drains to internal iliac nodes
- Inferior – drains to superficial inguinal lymph nodes.
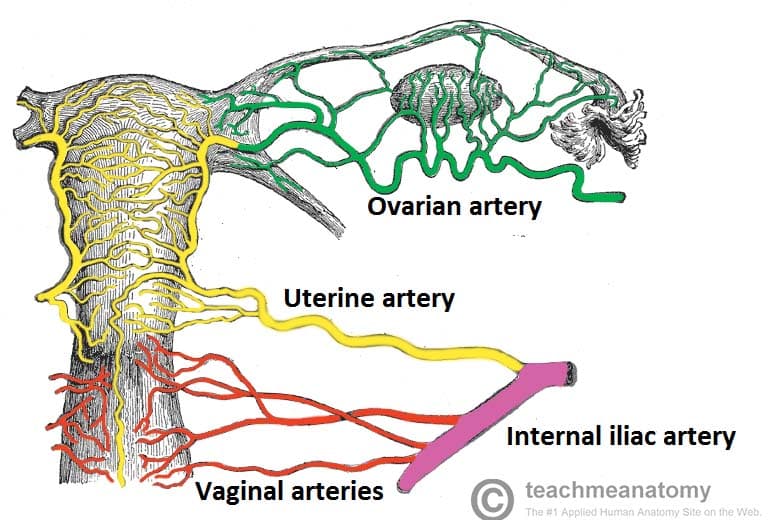
Fig 4 – Posterior view of the arterial supply to the female reproductive tract.
Innervation
Innervation is predominantly from the autonomic nervous system. Parasympathetic and sympathetic nerves arise from the uterovaginal nerve plexus (in turn a subsidiary of the inferior hypogastric plexus).
Only the inferior 1/5 of the vagina receives somatic innervation. This is via a branch of the pudendal nerve, the deep perineal nerve.
Clinical Relevance: Vaginal (Obstetric) Fistulae
A vaginal fistula is an open communication between the vagina and one of the adjacent pelvic organs.
It typically occurs as a result of prolonged labour (where a Caesarean section is not available). As the fetus slowly progresses down the vaginal wall, it exerts pressure – obstructing the blood supply and causing tissue necrosis.
There are three main types of vaginal fistulae:
- Vesicovaginal – abnormal communication with the bladder. Urine enters the vagina.
- Urethrovaginal – abnormal communication with the urethra. Urine only enters the vagina during urination.
- Rectovaginal – abnormal communication with the rectum. Faecal matter can enter the vagina.