The maxillary nerve is the second branch of the trigeminal nerve, which originates embryologically from the first pharyngeal arch.
Its primary function is sensory supply to the mid-third of the face.
In this article, we shall look at the anatomy of the maxillary nerve – its anatomical course, sensory and parasympathetic functions.
Anatomical Course
Trigeminal Nerve
The trigeminal nerve originates from four nuclei, which extend from the midbrain to the medulla (a nucleus refers to a collection of nerve cell bodies within the central nervous system):
- Three sensory nuclei:
- Mesencephalic nucleus
- Principle sensory nucleus
- Spinal nucleus
- Motor nucleus of the trigeminal nerve
At the level of the pons, the sensory nuclei merge to form a sensory root. The motor nucleus continues to form a separate motor root. These roots are analogous with the dorsal and ventral roots of the spinal cord.
Within the middle cranial fossa, the sensory root expands into the trigeminal ganglion (a ganglion refers to a collection of the nerve cell bodies outside the central nervous system).
The trigeminal ganglion is located lateral to the cavernous sinus, in a depression of the temporal bone known as the trigeminal cave or Meckel’s cave.
The motor root passes inferiorly to the sensory root, along the floor of the trigeminal cave. Motor fibres are only distributed to the mandibular division (V3).
From the trigeminal ganglion, the three terminal divisions of the trigeminal nerve arise; the ophthalmic (V1), maxillary (V2) and mandibular (V3) nerves.
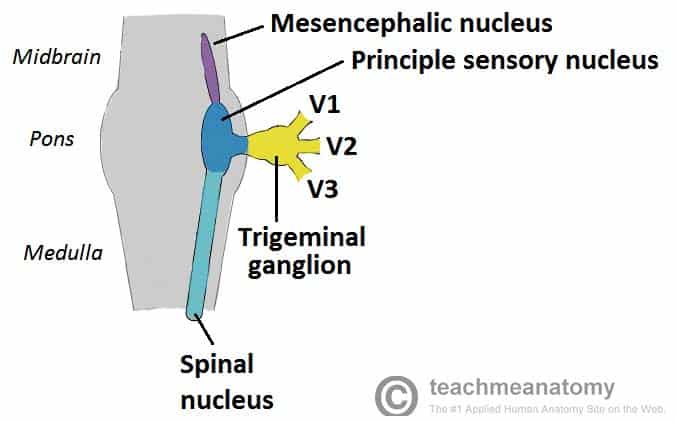
Fig 1 – The origin of the trigeminal nerve. Note that the nuclei are situated within in the CNS, and the gangia outside the CNS.
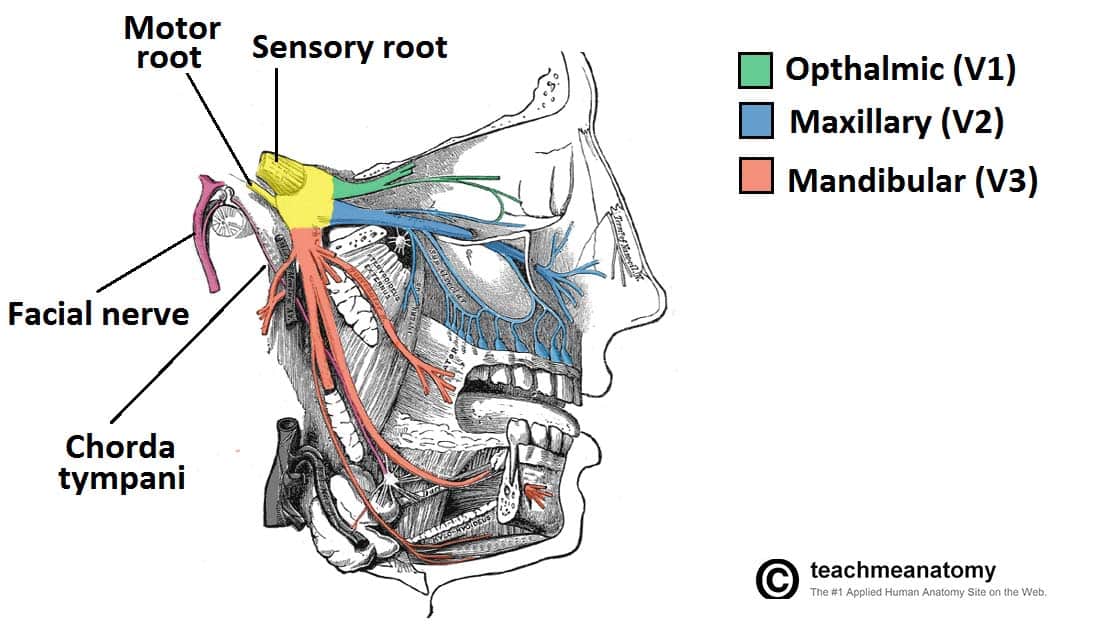
Fig 2 – Overview of the distribution of the trigeminal nerve and its terminal branches
Maxillary Nerve
After arising from the trigeminal ganglion, the maxillary nerve passes through the lateral wall of the cavernous sinus, before leaving the skull through the foramen rotundum. It gives rise to numerous sensory branches:
- Superior alveolar nerve (anterior, posterior and middle)
- Middle meningeal nerve
- Infraorbital nerve
- Zygomatic nerve
- Inferior palpebral nerve
- Superior labial nerve
- Pharyngeal nerve
- Greater and lesser palatine nerves
- Nasopalatine nerve
Sensory Function
The maxillary nerve’s terminal branches innervate the skin, mucous membranes and sinuses of derivatives of the maxillary prominence of the 1st pharyngeal arch:
- Lower eyelid and its conjunctiva
- Inferior posterior portion of the nasal cavity (superior anterior is CNV1)
- Cheeks and maxillary sinus
- Lateral nose
- Upper lip, teeth and gingiva
- Superior palate
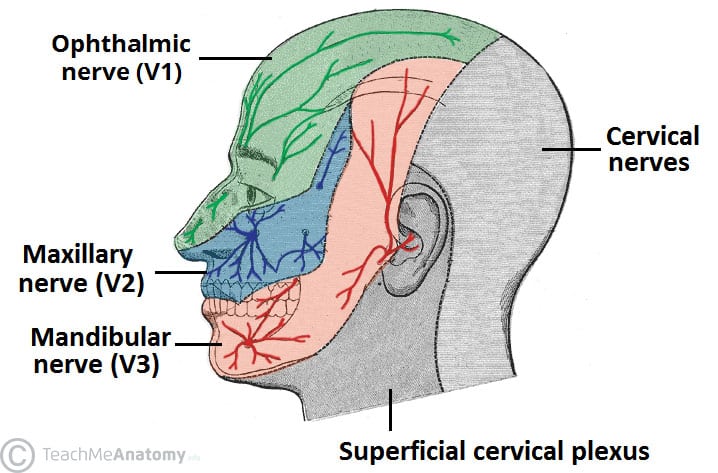
Fig 2.0 – Cutaneous distribution of the sensory supply of the maxillary nerve shown in blue.
Parasympathetic Function
Post ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve) travel with the maxillary nerve to:
- Lacrimal gland
- Mucous glands of the nasal mucosa
Clinical Relevance: Trigeminal Neuralgia
Trigeminal neuralgia is a disorder characterised by chronic pain over the trigeminal distribution of the face. This is an example of neuropathic pain, whereby there is damage to the nerves causing:
- Hyperalgesia – increased sensitivity to pain
- Allodynia – pain from a usually non-painful stimulus
As such, light touch can often trigger episodes of excruciating pain.
Its cause is unknown but it is thought to be the result of damage to trigeminal nerve due to conditions such as multiple sclerosis, stroke or trauma.
The pain is usually unresponsive to typical analgesics including opioids. As a result an anticonvulsant such as carbamazepine is often used to reduce nervous transmission of the pain by blocking active voltage gated sodium channels. If unresponsive to pharmacological agents, surgical destruction of the nerve is possible, but that understandably results in loss of sensation over the face.