The pudendal nerve is a major somatic nerve of the sacral plexus.
Overview:
- Nerve roots – S2-S4
- Sensory – innervates the external genitalia of both sexes and the skin around the anus, anal canal and perineum
- Motor – innervates various pelvic muscles, the external urethral sphincter and the external anal sphincter.
In this article, we shall look at the anatomy of the pudendal nerve – its course, motor and sensory functions, and any clinical correlations.
Anatomical Course
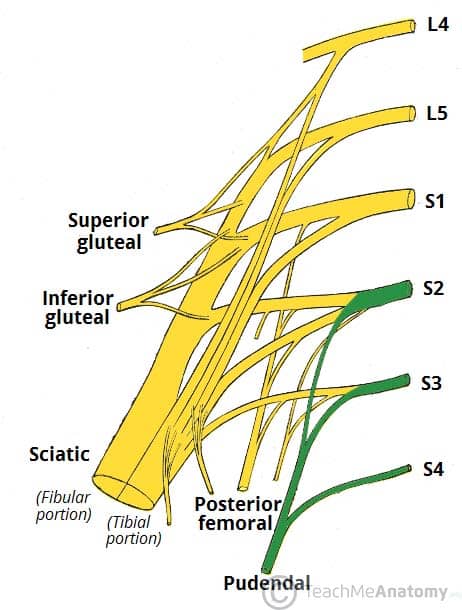
The pudendal nerve is formed from the sacral plexus – a network of nerve fibres located on the posterior pelvic wall. It arises from the ventral rami (anterior divisions) of the spinal nerves S2, S3 and S4.
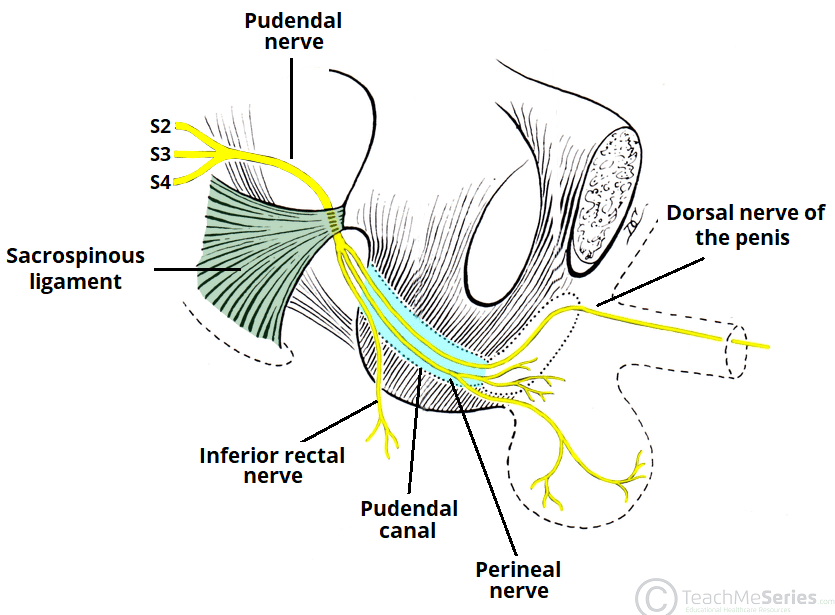
After its formation, the pudendal nerve descends and passes between the piriformis and ischiococcygeus muscles. It leaves the pelvis through the lower part of the greater sciatic foramen. It then crosses the sacrospinous ligament (close to its insertion to the ischial spine), and then re-enters the pelvis through the lesser sciatic foramen.
After re-entering the pelvis, it accompanies the internal pudendal artery and vein, coursing anterosuperiorly through the pudendal canal (also known as Alcock’s canal – a structure formed by the fascia of the obturator internus muscle). Inside the pudendal canal, the nerve divides into branches, first giving off the inferior rectal nerve, then the perineal nerve, before continuing as the dorsal nerve of the penis or clitoris.
Note: there is variation with the anatomical course between individuals, however, its close association to the ischial spine is generally consistent.
Motor Function
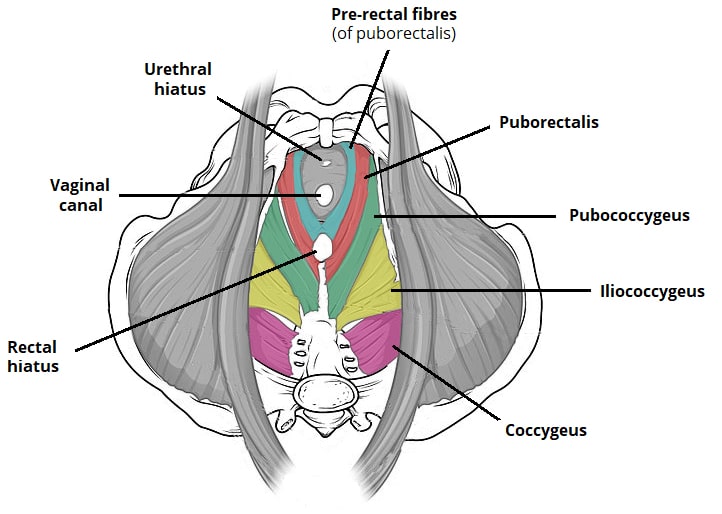
The perineal nerve innervates muscles of the perineum and pelvic floor:
- Bulbospongiosus
- Ischiocavernosus
- Levator ani muscles (including the iliococcygeus, pubococcygeus and puborectalis).
- The levator ani muscles also recieve innervation directly from the anterior ramus of the S4 nerve root
The nerve also innervates the external urethral sphincter. A branch of the pudendal nerve, the inferior rectal nerve, provides motor supply to the external anal sphincter. Therefore, the pudendal nerve provides the voluntary/somatic control of faecal and urinary continence.
(Tip: a way to remember the continence function of the pudendal nerve is; S2, S3, S4 keeps the poo off the floor!)
Sensory Function
The pudendal nerve supplies sensation to external genitalia of both sexes and the skin around the anus, anal canal and perineum through its branches:
- Inferior rectal nerve – innervates the perianal skin and lower third of the anal canal.
- Perineal nerve – innervates the skin of the perineum, labia minora and majora or posterior scrotum.
- Dorsal nerve of the penis or clitoris – innervates the skin of the penis or clitoris. Thus, responsible for the afferent component of penile and clitoral erection.
Clinical Relevance: Pudendal Nerve Block
A pudendal nerve block is a form of analgesia occasionally given before vaginal childbirth, episiotomy and other minor vaginal procedures.
To administer a pudendal nerve block, the patient is placed in the lithotomy position, and the ischial spine is palpated transvaginally. Local anaesthetic is then injected into the tissues around the ischial spine. The procedure is then completed on the opposite side.
As the pudendal nerve is accompanied by the internal pudendal artery, it is essential to aspirate before injecting local anaesthetic – this ensures that local anaesthetic is not administered into the systemic circulation.