The sciatic nerve is a major nerve of the lower limb. It is a thick flat band, approximately 2cm wide – the largest nerve in the body.
In this article, we shall look at the anatomy of the sciatic nerve – its anatomical course, motor and sensory functions, and its clinical correlations.
Overview
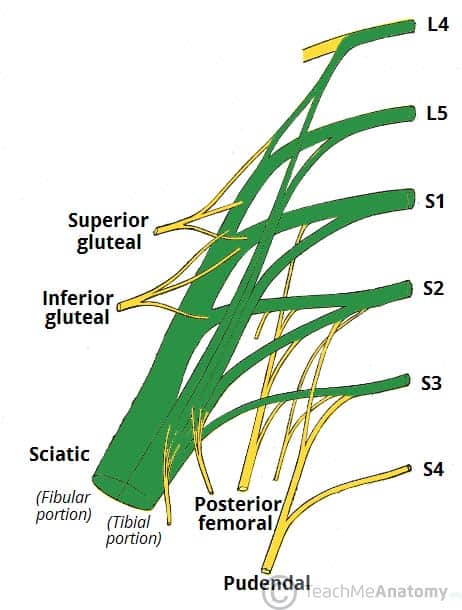
- Nerve roots: L4-S3.
- Motor functions:
- Innervates the muscles of the posterior thigh (biceps femoris, semimembranosus and semitendinosus) and the hamstring portion of the adductor magnus (remaining portion of which is supplied by the obturator nerve).
- Indirectly innervates (via its terminal branches) all the muscles of the leg and foot.
- Sensory functions: No direct sensory functions. Indirectly innervates (via its terminal branches) the skin of the lateral leg, heel, and both the dorsal and plantar surfaces of the foot.
Anatomical Course
The sciatic nerve is derived from the lumbosacral plexus. After its formation, it leaves the pelvis and enters the gluteal region via greater sciatic foramen. It emerges inferiorly to the piriformis muscle and descends in an inferolateral direction.
As the nerve moves through the gluteal region, it crosses the posterior surface of the superior gemellus, obturator internus, inferior gemellus and quadratus femoris muscles. It then enters the posterior thigh by passing deep to the long head of the biceps femoris.
Within the posterior thigh, the nerve gives rise to branches to the hamstring muscles and adductor magnus. When the sciatic nerve reaches the apex of the popliteal fossa, it terminates by bifurcating into the tibial and common fibular nerves.
Note: the sciatic nerve can be described as two individual nerves bundled together in the same connective tissue sheath – the tibial and common fibular nerves. These usually separate at the apex of the popliteal fossa, however in approximately 12% of people they separate as they leave the pelvis.
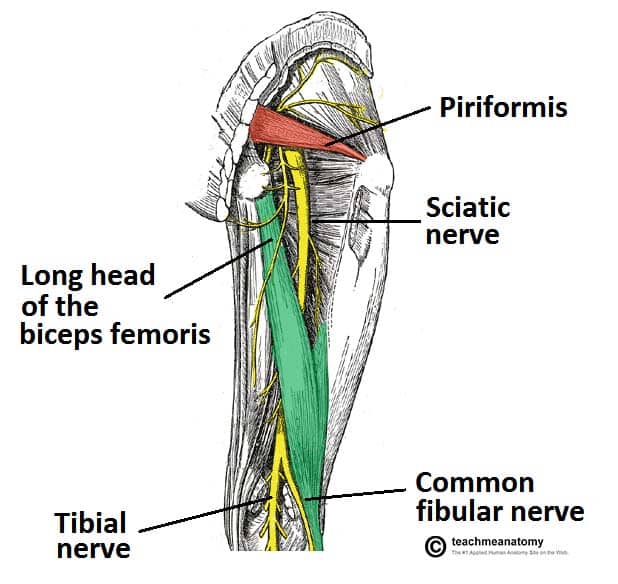
Fig 2 – View of the posterior thigh. The gluteus maximus and minimus have been removed to expose the sciatic nerve and underlying anatomical structures.
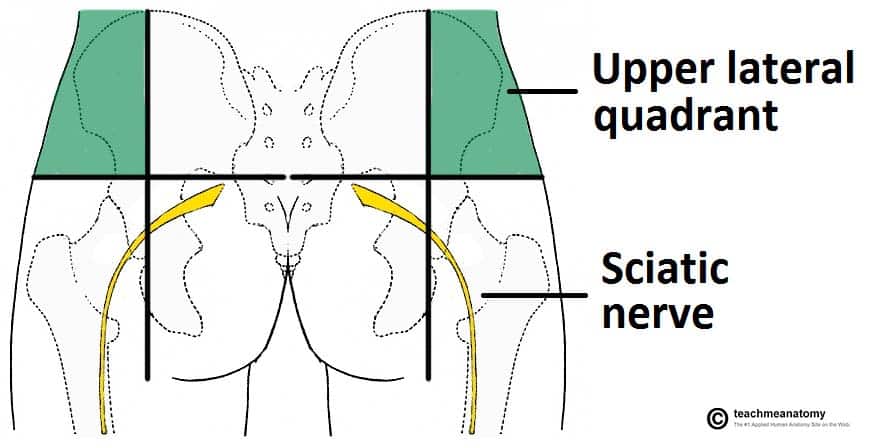
Clinical Relevance: Intramuscular Injections
The anatomical course of the sciatic nerve must be considered when administering intramuscular injections into the gluteal region. The region can be divided into quadrants using 2 lines, marked by bony landmarks:
- One line descends vertically from the highest point on the iliac crest.
- The other horizontal line passes through the vertical line half way between the highest point on the iliac crest and ischial tuberosity.
The sciatic nerve passes through the lower medial quadrant. To avoid damaging the sciatic nerve therefore, intramuscular injections are given only in the upper lateral quadrant of the gluteal region.
Motor Functions
Although the sciatic nerve passes through the gluteal region, it does not innervate any muscles there. However, the sciatic nerve does directly innervate the muscles in the posterior compartment of the thigh, and the hamstring portion of the adductor magnus.
The sciatic nerve also indirectly innervates several other muscles, via its two terminal branches:
- Tibial nerve – the muscles of the posterior leg (calf muscles), and some of the intrinsic muscles of the foot.
- Common fibular nerve – the muscles of the anterior leg, lateral leg, and the remaining intrinsic foot muscles.
In total, the sciatic nerve innervates the muscles of the posterior thigh, entire leg and entire foot.
Sensory Functions
The sciatic nerve does not have any direct cutaneous functions. It does provide indirect sensory innervation via its terminal branches:
- Tibial nerve – supplies the skin of the posterolateral leg, lateral foot and the sole of the foot.
- Common fibular nerve – supplies the skin of the lateral leg and the dorsum of the foot.

Fig 4 – The cutaneous innervation of the terminal branches of the sciatic nerve.
Clinical Relevance: Piriformis Syndrome
Piriformis syndrome refers to compression of the sciatic nerve by the piriformis muscle. It is also known as deep gluteal syndrome.
Clinical features include radicular pain, numbness, muscle weakness and buttock tenderness. The pain can occasionally be exacerbated by internal rotation of the lower limb at the hip.
X-ray and MRI imaging is usually unremarkable but can exclude other pathology such as spinal compression of the sciatic nerve.
The treatment of piriformis syndrome can be divided into non-operative and operative:
- Non-operative – analgesia, physiotherapy and corticosteroid injections
- Operative – piriformis muscle release