Bone is a specialised type of connective tissue. It has a unique histological appearance, which enables it to carry out its numerous functions:
- Haematopoiesis – the formation of blood cells from haematopoietic stem cells found in the bone marrow.
- Lipid and mineral storage – bone is a reservoir holding adipose tissue within the bone marrow and calcium within the hydroxyapatite crystals.
- Support – bones form the framework and shape of the body.
- Protection – especially the axial skeleton which surrounds the major organs of the body.
In this article, we shall look at the ultrastructure of bone – its components, structure and development. We shall also examine how disease can affect its structure.
Components of Bone
Bone is a specialised form of connective tissue. Like any connective tissue, its components can be divided into cellular components and the extracellular matrix.
Cellular Components
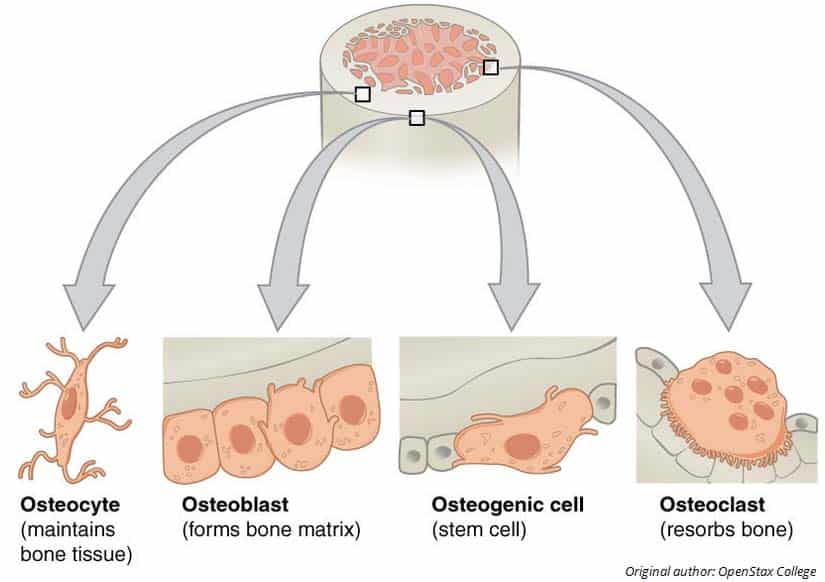
There are three types of cells in bone:
- Osteoblasts – Synthesise uncalcified/unmineralised extracellular matrix called osteoid. This will later become calcified/mineralised to form bone.
- Osteocytes – As the osteoid mineralises, the osteoblasts become entombed between lamellae in lacunae where they mature into osteocytes. They then monitor the minerals and proteins to regulate bone mass.
- Osteoclasts – Derived from monocytes and resorb bone by releasing H+ ions and lysosomal enzymes. They are large and multinucleated cells.
The balance of osteoblast to osteoclast activity is crucial in the maintenance of the tissue’s structural integrity. It also plays a role in conditions such as osteoporosis.
Extracellular Matrix
The extracellular matrix (ECM) refers to the molecules that provide biochemical and structural support to the cells.
The ECM of bone is highly specialised. In addition to collagen and the associated proteins usually found in connective tissue, bone is impregnated with mineral salts, in particular calcium hydroxyapatite crystals. These crystals associate with the collagen fibres, making bone hard and strong. This matrix is organised into numerous thin layers, known as lamellae.
Structure of Bone
Under the microscope, bone can be divided into two types:
- Woven bone (primary bone) – Appears in embryonic development and fracture repair, as it can be laid down rapidly. It consists of osteoid (unmineralised ECM), with the collagen fibres arranged randomly. It is a temporary structure, soon replaced by mature lamellar bone.
- Lamellar bone (secondary bone) – The bone of the adult skeleton. It consists of highly organised sheets of mineralised osteoid. This organised structure makes it much stronger than woven bone. Lamella bone itself can be divided into two types – compact and spongy.
In both types of bone, the external surface is covered by a layer of connective tissue, known as the periosteum. A similar layer, the endosteum lines the cavities within bone (such as the medullary canal, Volkmann’s canal and spongy bone spaces).
Lamellar bone can be divided into two types. The outer is known as compact bone – this is dense and rigid. The inner layers of bone are marked by many interconnecting cavities and is called spongy bone.
Compact Bone
Compact bone forms the outer ‘shell’ of bone. In this type of bone, the lamellae are organised into concentric circles, which surround a vertical Haversian canal (which transmits small neurovascular and lymphatic vessels). This entire structure is called an osteon and is the functional unit of bone.
The Haversian canals are connected by horizontal Volkmann’s canals – these contain small vessels that anastomose (join) with the arteries of the Haversian canals. The Volkmann’s canals also transmit blood vessels from the periosteum.
Osteocytes are located between the lamellae, within small cavities (known as lacunae). The lacunae are interconnected by a series of interconnecting tunnels, called canaliculi.
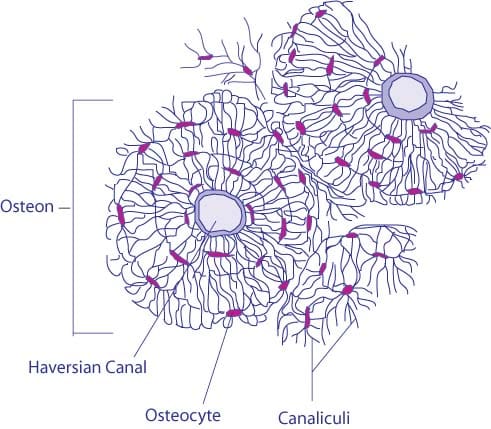
Fig 2 – Micrograph of compact bone. Note the arrangement around a single Haversian canal.
Spongy Bone
Spongy bone makes up the interior of most bones and is located deep to the compact bone. It contains many large spaces – this gives it a honeycombed appearance.
The bony matrix consists of a 3D network of fine columns, which crosslink to form irregular trabeculae. This produces a light, porous bone, that is strong against multidirectional lines of force. The lightness afforded to spongy bone is crucial in allowing the body to move. If the only type of bone was compact, they would be too heavy to mobilise.
The spaces between trabeculae are often filled with bone marrow. Yellow bone marrow contains adipocytes and red bone marrow consists of haematopoietic stem cells.
This type of bone does not contain any Volkmann’s or Haversian canals.
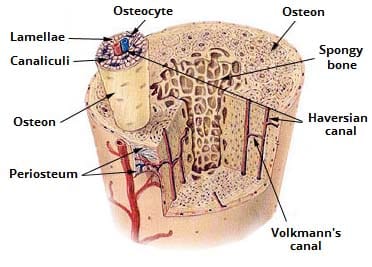
Fig 3 – Structure of mature bone. Note the differing structure of compact and spongy bone types.
Ossification and Remodelling
Ossification is the process of producing new bone. It occurs via one of two mechanisms:
- Endochondral ossification – Where hyaline cartilage is replaced by osteoblasts secreting osteoid. The femur is an example of a bone that undergoes endochondral ossification.
- Intramembranous ossification – Where mesenchymal (embryonic) tissue is condensed into bone. This type of ossification forms flat bones such as the temporal bone and the scapula.
In both mechanisms, primary bone is initially produced. It is later replaced by mature secondary bone.
Remodelling
Bone is a living tissue and as such constantly undergoes remodelling. This is the process whereby mature bone tissue is reabsorbed, and new bone tissue is formed. It is carried out by the cellular component of bone.
Osteoclasts break down bone via a cutting cone. The nutrients are reabsorbed, and osteoblasts lay down new osteoid. Remodelling occurs primarily at sites of stress and damage, strengthening the areas affected.
Clinical Relevance – Disorders of Bone
Bone has a unique histological structure, which is required for it to carry out its functions. Alterations to this structure, secondary to disease, can give rise to several clinical conditions.
Osteogenesis imperfecta is a condition in which there is abnormal synthesis of collagen from the osteoblasts. Clinical features include fragile bones, bone deformities and blue sclera. It is a rare disease and genetic in aetiology, with an autosomal dominant inheritance pattern. The fragility of the bones predisposes them to fracture – this has a medicolegal importance, as in children it can be mistaken for deliberate injury.
Osteoporosis refers to a decrease in bone density, reducing its structural integrity. This is produced by osteoclast activity (bone reabsorption) outweighing osteoblast activity (bone production). The bones are fragile, and at an increased risk of fracture. There are three types:
- Type 1: Postmenopausal osteoporosis – Develops in women after the menopause, due to decreased oestrogen production. Oestrogen protects against osteoporosis by increasing osteoblast and decreasing osteoclast activity.
- Type 2: Senile osteoporosis – Usually occurs above the age of 70.
- Type 3: Secondary osteoporosis – Where osteoporosis occurs due to co-existing disease (e.g. chronic renal failure).
Risk factors include age, gender, diet (vitamin D and calcium), ethnicity, smoking and immobility. It is usually managed by bisphosphonates which are taken up by osteoclasts causing them to become inactive and undergo apoptosis. This limits further degradation of bone.
Rickets is Vitamin D or calcium deficiency in children with growing bones. This means that the osteoid mineralises poorly and remains pliable. The epiphyseal growth plates can then become distorted under the weight of the body, potentially leading to skeletal deformities.
Osteomalacia is a Vitamin D or calcium deficiency in adults with remodelling bones. Here the osteoid laid down by osteoblasts is poorly mineralised leading to increasingly weak bones, increasing their susceptibility to fracture.
Note: Vitamin D deficiency can be due to poor diet, lack of sunlight or a metabolic disorder. For example, kidney failure could interfere with the second hydroxylation of vitamin D or an intestinal disorder may prevent sufficient absorption. A calcium deficiency can be caused by diet or low vit. D.