The ophthalmic nerve (CNV1) is a terminal branch of the trigeminal nerve (along with the maxillary and mandibular nerves).
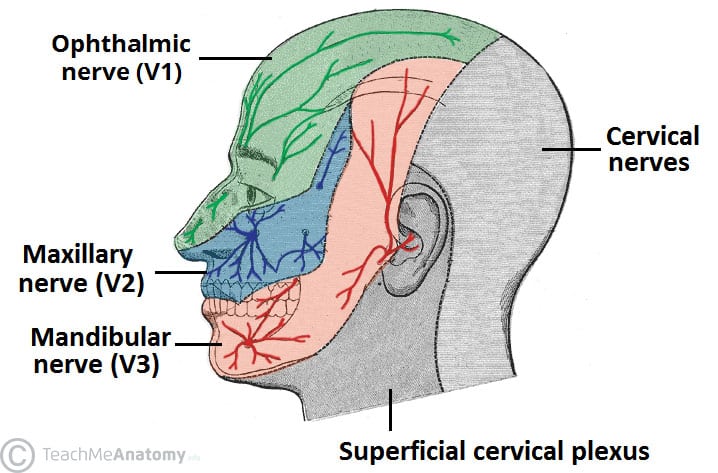
It provides sensory innervation to the skin, mucous membranes and sinuses of the upper face and scalp.
In this article, we will look at the anatomy of the ophthalmic nerve – its anatomical course, sensory functions and autonomic functions.
Anatomical Course
Trigeminal Nerve
The trigeminal nerve originates from four nuclei, which extend from the midbrain to the medulla (a nucleus refers to a collection of nerve cell bodies within the central nervous system):
- Three sensory nuclei:
- Mesencephalic nucleus
- Principle sensory nucleus
- Spinal nucleus
- Motor nucleus of the trigeminal nerve
At the level of the pons, the sensory nuclei merge to form a sensory root. The motor nucleus continues to form a separate motor root. These roots are analogous with the dorsal and ventral roots of the spinal cord.
Within the middle cranial fossa, the sensory root expands into the trigeminal ganglion (a ganglion refers to a collection of the nerve cell bodies outside the central nervous system).
The trigeminal ganglion is located lateral to the cavernous sinus, in a depression of the temporal bone known as the trigeminal cave or Meckel’s cave.
The motor root passes inferiorly to the sensory root, along the floor of the trigeminal cave. Motor fibres are only distributed to the mandibular division (V3).
From the trigeminal ganglion, the three terminal divisions of the trigeminal nerve arise; the ophthalmic (V1), maxillary (V2) and mandibular (V3) nerves.
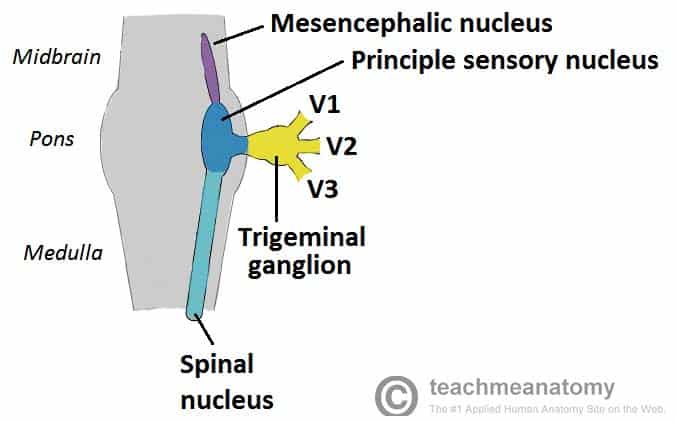
Fig 1 – The origin of the trigeminal nerve. Note that the nuclei are situated within in the CNS, and the gangia outside the CNS.
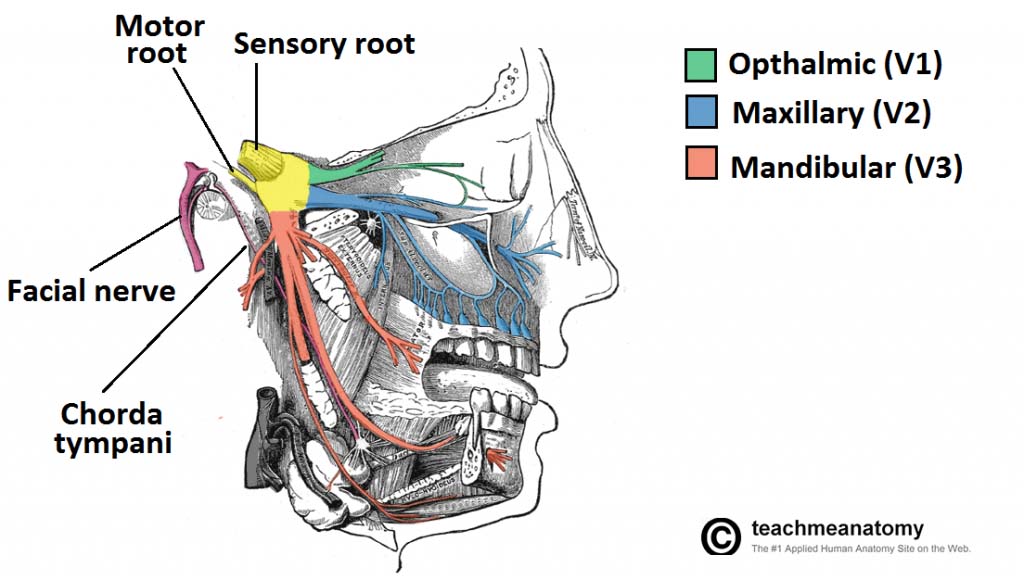
Fig 2 – Overview of the distribution of the trigeminal nerve and its terminal branches
Ophthalmic Nerve
After arising from the trigeminal ganglion, the ophthalmic nerve travels laterally to the cavernous sinus and gives rise to the recurrent tentorial branch (which supplies the tentorium cerebelli).
The nerve then then exits the cranium via the superior orbital fissure, where it divides into its three main branches:
- Frontal nerve
- Lacrimal nerve
- Nasociliary nerve
These three branches provide sensory innervation to the skin and mucous membranes of the structures derived from the frontonasal prominence.
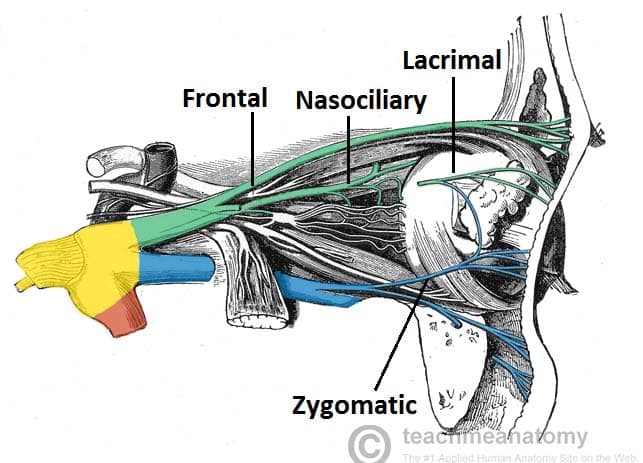
Fig 3 – Nervous supply to the orbit from the ophthalmic and maxillary nerves (other nerves. e.g. orbital not labelled)
Sensory Function
The ophthalmic division of trigeminal nerve provides sensory innervation to the following structures:
- Forehead and scalp
- Frontal, ethmoid and sphenoid sinuses
- Upper eyelid and its conjunctiva
- Cornea
- Dorsum of the nose
- Lacrimal gland
- Parts of the meninges and tentorium cerebelli (recurrent tentorial branch)
The table below outlines the structures innervated by branches of CNV1.
| Nerve | Branches | Innervation |
| Frontal (largest of three terminal branches of CNV1) | Supraorbital | Upper eyelid and conjunctiva
Scalp |
| Supratrochlear | Upper eyelid and conjunctiva
Forehead |
|
| Lacrimal (smallest of three terminal branches of CNV1) | Receives branch from zygomatic nerve of CNV2 containing parasympathetic fibres | Sensory innervation of lacrimal gland, upper eyelid and conjunctiva
Contains parasympathetic fibres to lacrimal gland. |
| Nasociliary | Anterior ethmoid nerve | Sensory innervation of mucous membranes of frontal, ethmoid and sphenoid sinuses.
Nasal cavity |
| Posterior ethmoid nerve | Absent in approximately 30% of people
Sensory innervation to mucous membranes of sphenoid sinus |
|
| Infratrochlear nerve | Bridge of nose Upper eyelid and conjunctiva | |
| Long ciliary nerves | Sensory innervation to eye (cornea, ciliary bodies, iris)
Contains sympathetic fibres to dilator pupillae muscle. |
Mapping Cutaneous Innervation
The cutaneous innervation to the face and scalp by the three branches of the trigeminal nerve have sharp borders and little overlap. The cutaneous innervation of CNV1 can be seen in the image below:
Autonomic Functions
The ophthalmic nerve itself does not contain any autonomic fibres. However, nerves from the sympathetic and parasympathetic system ‘hitchhike’ on CNV1:
- Sympathetic fibres (from the superior cervical ganglion) hitchhike on branches of the nasociliary nerve (long ciliary nerves) to reach the dilator pupillae in the eye.
- Parasympathetic fibres (from the pterygopalatine ganglion) hitchhike along the zygomatic branch of the maxillary nerve (CNV2) and then the lacrimal branch of the ophthalmic nerve (CNV1) to reach the lacrimal gland. The lacrimal branch itself provides sensory innervation to the lacrimal gland.
Clinical Relevance: Corneal Reflex
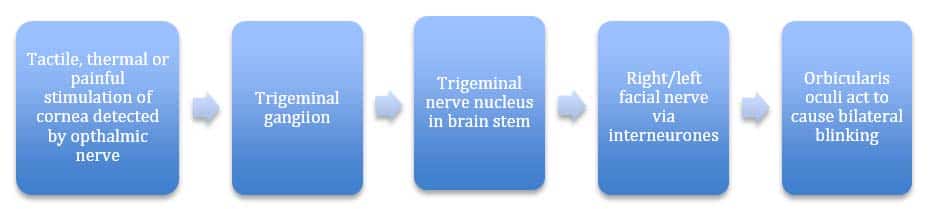
The corneal reflex is the involuntary blinking of the eyelids – stimulated by tactile, thermal or painful stimulation of the cornea.
In the corneal reflex, the ophthalmic nerve acts as the afferent limb – detecting the stimuli. The facial nerve is the efferent limb, causing contraction of the orbicularis oculi muscle.
If the corneal reflex is absent, it is a sign of damage to the trigeminal/ophthalmic nerve or the facial nerve.