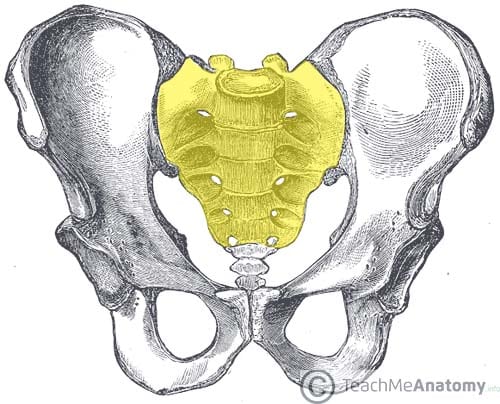
The sacrum is a large bone located at the terminal part of the vertebral canal, where it forms the posterior aspect of the pelvis. It is remarkably thick, which aids in supporting and transmitting the weight of the body.
In this article we will look at the anatomy of the sacrum – its gross structure, muscular and ligamentous attachments, neighbouring neurovasculature, as well as some relevant clinical notes.
Bony Landmarks
The sacrum is formed by the fusion of the five sacral vertebrae. It has an inverted triangular, concave shape. The bone consists of a base, apex and four surfaces:
- Base – articulates superiorly with the fifth lumbar vertebra and its associated intervertebral disc.
- Apex – abuts the coccyx inferiorly.
- Auricular surfaces – located laterally on the sacrum, and shaped like the outer ear – hence the name. Each articulates with the auricular surface of the ilium.
- Anterior and posterior surfaces – provide attachment to pelvic ligaments and muscles.
Internally, the central canal of the vertebral column continues along the core of the sacrum and ends at the 4th sacral foramina, as the sacral hiatus.
Surfaces of the Sacrum
There are two surfaces of the sacrum – a coarse dorsal surface and a relatively smooth pelvic surface. When the patient is standing, the pelvic surface faces anteroinferiorly while the dorsal surface is in the posterosuperior direction.
Dorsal Surface
The dorsal surface of the sacrum is coarse and rugged. This can be attributed to the fusion of the sacral vertebrae, which give rise to three bony ridges (or crests).
In the midline of the dorsal surface, there is a central ridge of bone, called the median sacral crest. It is formed by the fusion of the spinous processes of the first three sacral vertebrae. It gives attachment to the supraspinous ligament.
The intermediate sacral crests are formed by the fusion of the sacral articular processes. The posterior sacroiliac ligaments are attached along this crest. It should be noted that the superior articulating process of S1 and the inferior articulating process of S5 are not fused. Therefore, the former articulates with the inferior articulating process of L5, while the latter – also known as the sacral cornu – articulates with the coccygeal cornu (superior articulating process of coccyx).
Finally, the transverse processes of the five sacral bones fuse to form the lateral sacral crests, which offers a point of attachment to the posterior sacroiliac ligaments as well as the sacrotuberous ligament. The fusion of these processes is not complete, allowing the sacral nerve fibres to enter and leave the central canal by way of the four pairs of posterior sacral foramina.
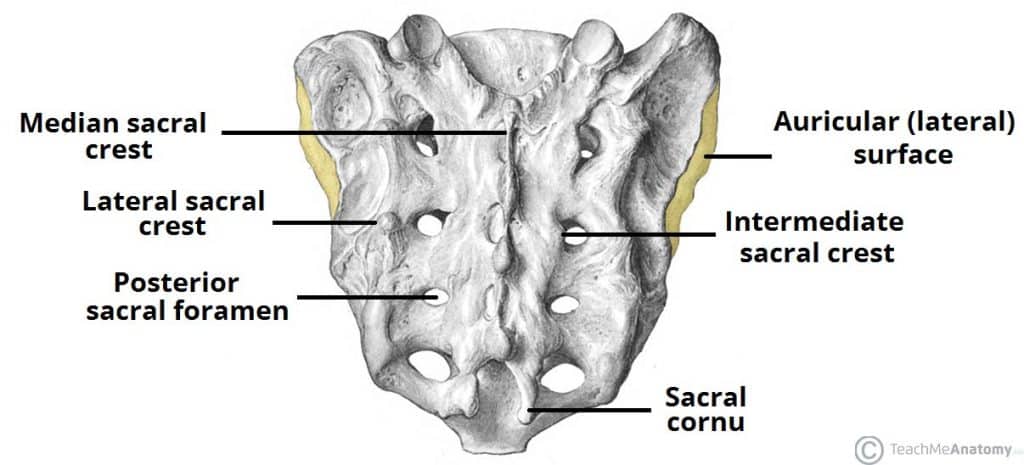
Fig 2 – The posterior surface of the sacrum. The lateral surfaces are also partially visible.
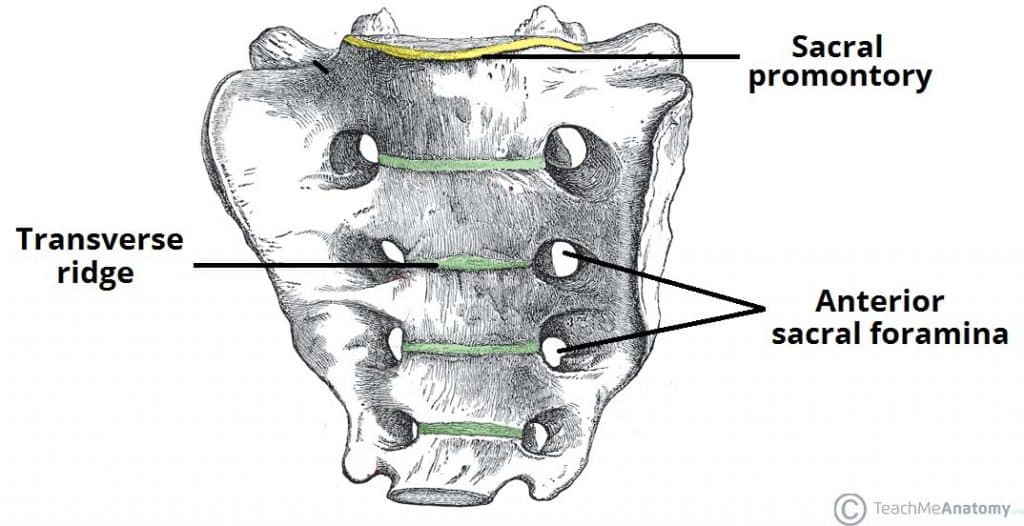
Pelvic Surface
The pelvic surface of the sacrum is less remarkable than the dorsal surface. In the adult, the surface is marked by four transverse lines – the remnants of the fused sacral intervertebral discs (fusion of the sacral vertebrae begins at age 20).
Superiorly, there is an anterior projection of bone, known as the sacral promontory. It forms the posterior margin of the pelvic inlet and as a result, it is serially continuous with the margin of the ala of the sacrum, arcuate line of the ilium, and the pectin pubis and pubic crest of the pubic bone.
Clinical Relevance: Sexual Dimorphism of the Pelvis
The sacrum contributes to the sexual dimorphism of the pelvis. Firstly, the sacral promontory is less prominent in females than in males. This results in an oval-shaped pelvic inlet in females and a heart-shaped pelvic inlet in males.
Additionally, a smaller promontory results in a wider anteroposterior – both true conjugate (from the top of the symphysis pubis to the promontory) and diagonal conjugate (from subpubic angle to promontory) – measurement. The wider space permits the passage of child during delivery.
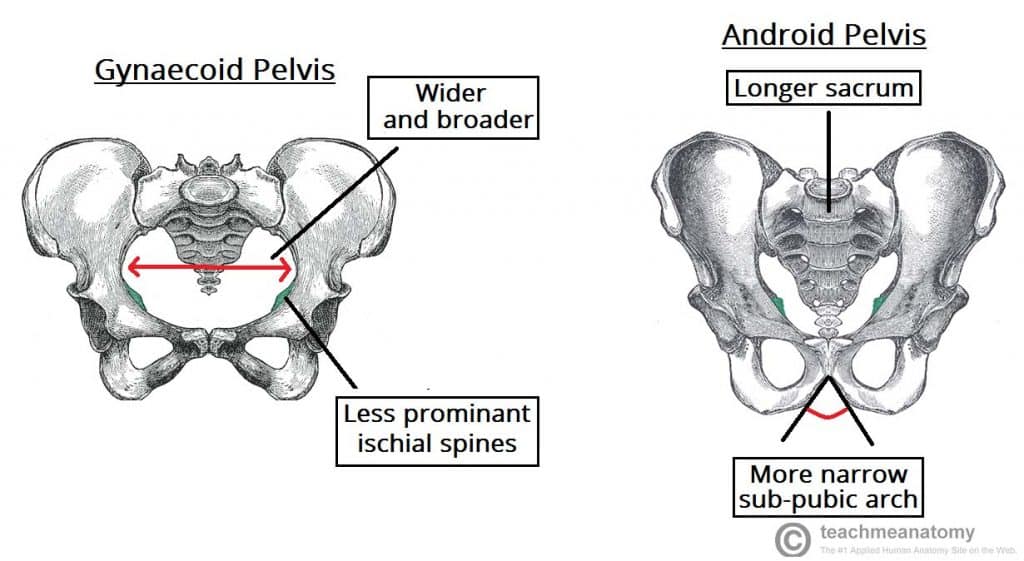
Fig 4 – Comparing the gynaecoid (female) pelvis with the android (male) pelvis.
Muscular Attachments
Both the anterior and posterior surfaces of the sacrum serve as points of origin or attachment for several lower limb and back muscles. They can be divided into the those that are associated with the anterior surface, and those associated with the posterior surface.
Anterior Surface
- Piriformis: Originates from S2 – S4 level of the pelvic surface. Due to its attachment at the trochanter of the femur, it is able to externally rotate, abduct, extend and stabilise the hip joint.
- Coccygeus muscle inserts on the lower sacrum. It gives support to the contents of the pelvic cavity and due to its attachment to the coccyx, is able to flex the bone.
- Iliacus – although it primarily arises from the iliac fossa, it also has fibres originating at the ala of the sacrum. Its distal attachment to the lesser trochanter of the femur allows it to flex the thigh at the hips and stabilize the hip joint.
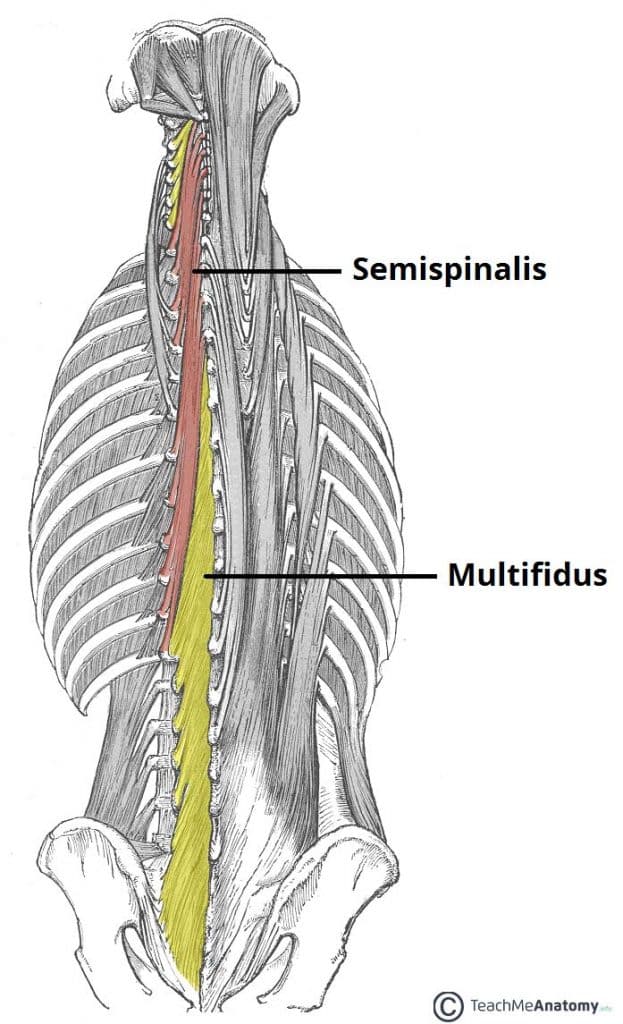
Posterior Surface
- Multifidus lumborum – the deepest muscle arising from the sacrum. Some of its fibres cover the upper two sacral foramina. This muscle attaches to the transverse processes of the superior vertebrae and is therefore able to help stabilize the spine.
- Erector spinae – partly arises from the posterior sacrum and the sacrospinous ligament. It is essential in achieving extension and lateral bending of the head and vertebral column.
Neurovascular Relations
As part of the pelvic girdle and vertebral column, the sacrum lies in close proximity to several important structures.
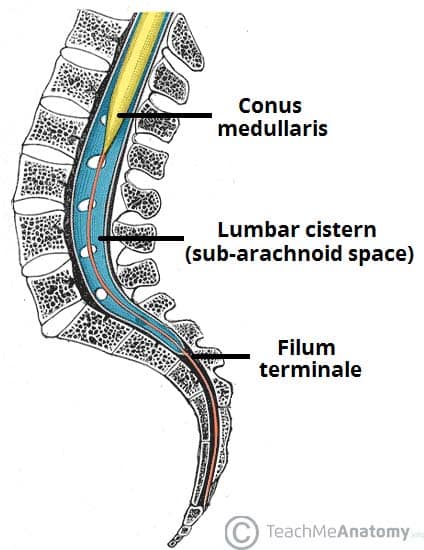
Spinal Cord
The central canal of the sacrum is home to the sacral fibres of the cauda equina (a bundle of spinal nerves that arise from the terminus of the spinal cord). The proximal parts of these fibres are contained within the dural sac, which terminates at about the level of S2.
The filum terminale (a continuation of the pia mater from the conus medullaris of the spinal cord) is joined by the arachnoid and dura mater at the level of S2 and continues inferiorly through the sacrum as the coccygeal ligament to its attachment at the coccyx.
Autonomic
The sacral part of the two sympathetic trunks run along the pelvic surface of the sacrum, medial to the sacral foramina. Each trunk has four ganglia in this region.
Vasculature
The median and lateral sacral arteries share a close anatomical relationship with the sacrum:
- Median sacral artery – has a midline relation to the sacrum. It is a continuation of abdominal aorta that arises posteriorly before its bifurcation. The artery runs along midline to the coccyx while supplying the posterior rectum, glomus coccygeum (coccygeal gland), and anastomosing with the lateral sacral arteries and supply meninges and sacrum along the way.
- Lateral sacral arteries – a pair of bilateral vessels that runs along the medial border of the sacral foramina. They arise from the posterior division of internal iliac artery and give rise to superior and inferior branches. Like the median artery, they also supply the meninges, sacrum and surrounding muscles.
References
Written by Lorenzo Crumbie, Writer at Kenhub.
Netter, F. (2014). Atlas of Human Anatomy. 6th ed. Philadelphia, PA: Elsevier: Saunders, pp.157-158, 160, 161, 167, 332-334, 477-478.
Sinnatamby, C. and Last, R. (2011). Last’s Anatomy. 12th ed. Edinburgh: Churchill Livingstone/Elsevier, pp.323-324.