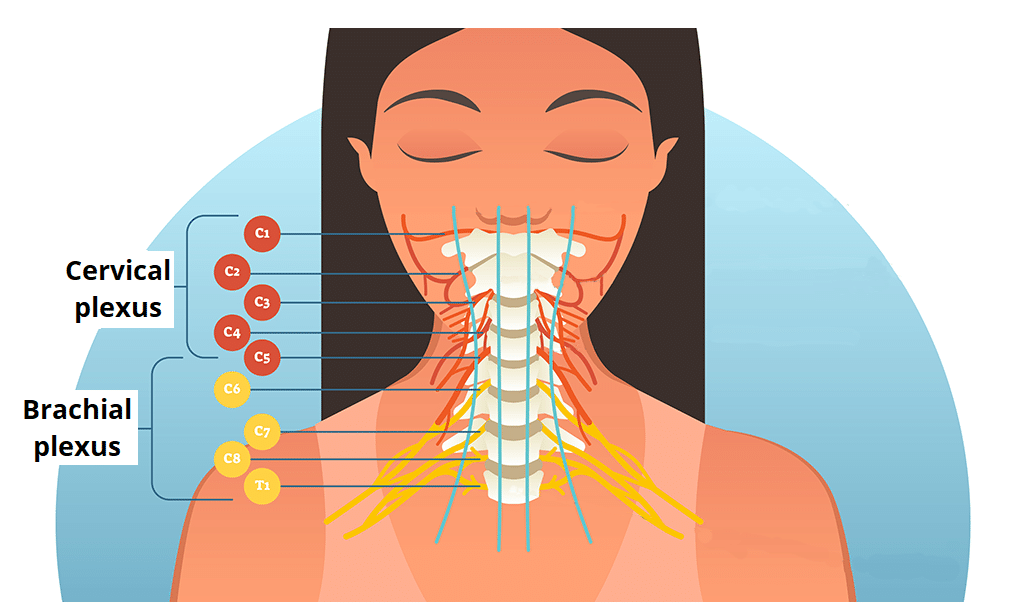
The cervical plexus is a network of nerve fibres that supplies innervation to some of the structures in the neck and trunk.
It is located in the posterior triangle of the neck, halfway up the sternocleidomastoid muscle, and within the prevertebral layer of cervical fascia. The plexus is formed by the anterior rami (divisions) of cervical spinal nerves C1-C4.
In this article, we shall look at the anatomy of the cervical plexus – its branches, functions and clinical correlations.
Spinal Nerves
The spinal nerves C1 – C4 form the basis of the cervical plexus.
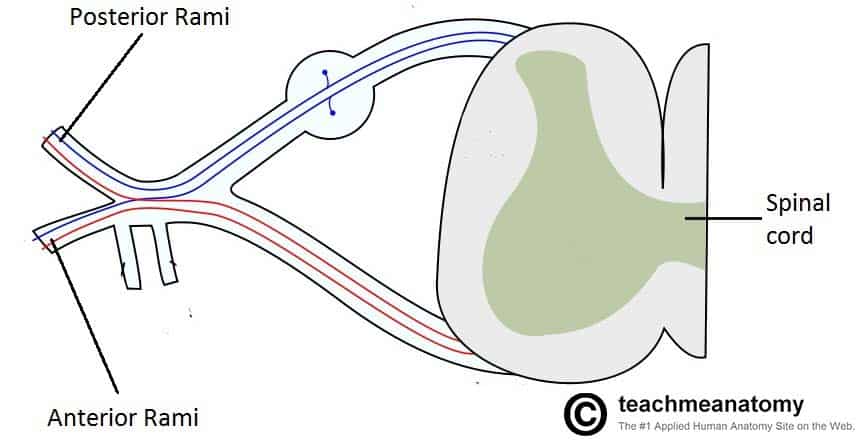
At each vertebral level, paired spinal nerves leave the spinal cord via the intervertebral foramina of the vertebral column.
Each nerve then divides into anterior and posterior nerve fibres. The cervical plexus begins as the anterior fibres of the spinal nerves C1, C2, C3 and C4.
These fibres combine with each other to form the branches of the cervical plexus.
Branches of the Cervical Plexus
The cervical plexus gives rise to numerous branches which supply structures in the head and neck. They can broadly be divided into two groups – muscular branches and sensory branches.
We shall now examine these branches in more detail.
Muscular Branches
The muscular branches of the cervical plexus are located deep to the sensory branches. They supply some of the muscles of the neck, back and the diaphragm.
After arising from the cervical plexus, the muscular branches tend to travel initially in an anteromedial direction. This is in contrast to the cutaneous branches, which travel posteriorly.
Phrenic Nerve
The phrenic nerve arises from the anterior rami of C3-C5. It provides motor innervation to the diaphragm.
After arising from the cervical plexus, the nerve travels down the surface of the anterior scalene muscle and enters the thorax. In the thoracic cavity, the nerve descends anteriorly to the root of the lung to reach the diaphragm.
A good memory aid for the roots of the phrenic nerve is C3,4,5 keeps the diaphragm alive.
Nerves to Geniohyoid and Thyrohyoid
The C1 spinal nerve gives rise to nerves to the geniohyoid (moves the hyoid bone anteriorly and upwards, expanding the airway) and the thyrohyoid (which depresses the hyoid bone and elevates the larynx).
These nerves travel with the hypoglossal nerve to reach their respective muscles.
Ansa Cervicalis
The ansa cervicalis is a loop of nerves, formed by nerve roots C1-C3. It gives off four muscular branches:
- Superior belly of the omohyoid muscle
- Inferior belly of omohyoid muscle
- Sternohyoid
- Sternothyroid
These muscles (the infrahyoids) act to depress the hyoid bone; an important function for swallowing and speech.
Other Muscular Branches
Several other minor branches arise from the nerve roots to supply muscles of the neck and back:
- C1-C2: Rectus capitis anterior and lateralis
- C1-C3: Longus capitis
- C2-C3: Contributions to the prevertebral muscles and sternocleidomastoid
- C3-C4: Contributions to the levator scapulae, trapezius and scalenus medius
The middle and anterior scalenus muscles also receive innervation directly from the cervical plexus.
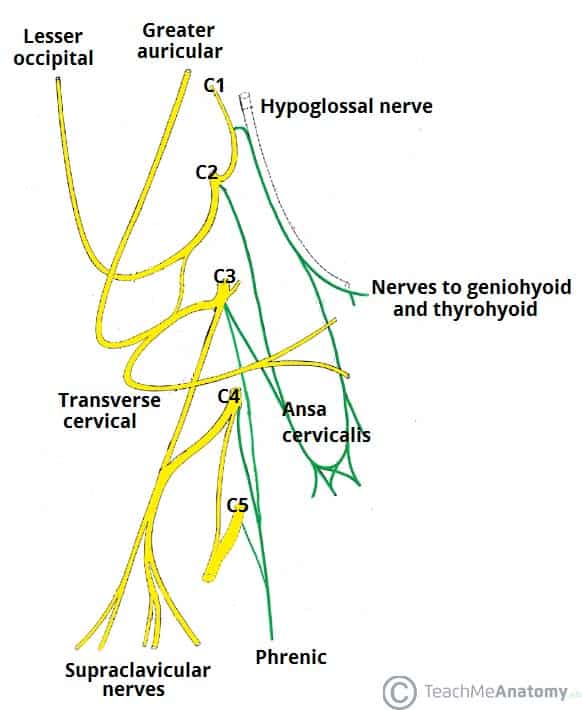
Fig 3 – The branches of the cervical plexus. The smaller branches have been removed for simplicity.
Sensory Branches
The cutaneous branches of the cervical plexus supply the skin of the neck, upper thorax, scalp and ear. These nerves all enter the skin at the middle of the posterior border of the sternocleidomastoid. This area is known as the nerve point of the neck (Erb’s point), and is utilised when performing a cervical plexus nerve block.
Greater Auricular Nerve
The greater auricular nerve is formed by fibres from C2 and C3 roots. It provides sensation to the external ear and the skin over the parotid gland. It is the largest ascending branch of the plexus.
The nerve also communicates with the auricular branch of the vagus nerve and the posterior auricular branch of the facial nerve (which innervates some small muscles around the ear).
Transverse Cervical Nerve
The transverse cervical nerve is also formed by fibres from C2 and C3. It curves around the posterior aspect of the sternocleidomastoid, and supplies sensation to the anterior neck. The nerve then pierces the deep cervical fascia and then gives branches that pass superiorly and inferiorly to supply the anterolateral skin of the neck and upper sternum.
Lesser Occipital Nerve
The lesser occipital nerve is derived from the C2 root, with a contribution from C3 in some individuals. It supplies cutaneous sensation to the posterosuperior scalp, and commonly communicates with the posterior branch of the greater auricular nerve.
After its formation, the nerve curves around the accessory nerve, and passes superiorly, close to the posterior border of the sternocleidomastoid.
Supraclavicular Nerves
The supraclavicular nerves are a group of nerves formed from the C3 and C4 roots.
They arise from the behind the posterior border of sternocleidomastoid, and provide sensation to the skin overlying the supraclavicular fossa and upper thoracic region and sternoclavicular joint.
Clinical Relevance – Cervical Plexus Block
A cervical plexus block is used to provide regional anaesthesia, usually for surgery in the neck region – such as carotid endarterectomy, thyroidectomy and cervical lymph node excision.
The anaesthetist inserts the needle containing the local anaesthetic, midway up the posterior border of the sternocleidomastoid (the nerve point of the neck). They then proceed to inject three times in a fan like fashion, with the needle pointing cranially, caudally and then anteriorly.
Note: as this procedure can also affect the phrenic nerve, it is usually not performed on those with co-existing cardiac or respiratory disease.
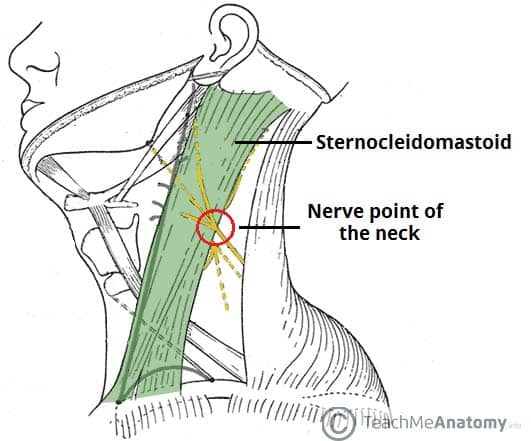
Fig 4 – The nerve point of the neck, where many cutaneous branches emerge.