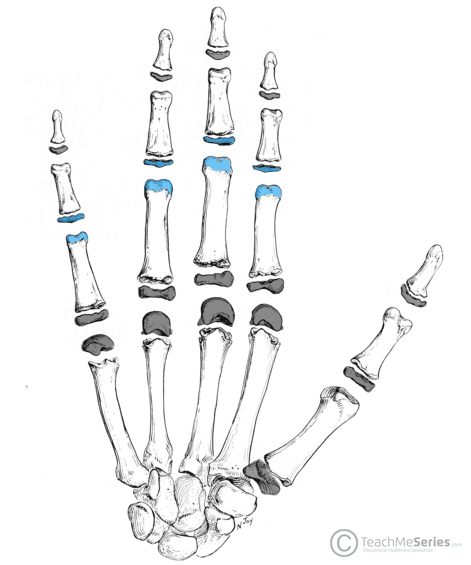
The proximal interphalangeal joint (PIPJ) refers to the articulation between the proximal and middle phalanx in the hand. It is present in all digits except the thumb.
It is a synovial hinge joint which permits flexion and extension in center of the fingers, contributing to fine motor control.
In this article, we shall look at the anatomy of the proximal interphalangeal joint – its structure, neurovascular supply, and clinical correlations.
Anatomical Structure
Articulating Surfaces
The proximal interphalangeal joint is formed by the articulation between the head of the proximal phalanx and the base of the middle phalanx:
- Head of the proximal phalanx – formed by two curved condylar processes, which form a shallow groove in the middle.
- Base of the middle phalanx – formed by two opposing concave sections which form a raised ridge. This ridge fits neatly into the proximal groove and provides great intraarticular stability.
Joint Capsule
Each proximal interphalangeal joint is surrounded by a small fibrous capsule. It is lined by a synovial membrane and filled with synovial fluid.
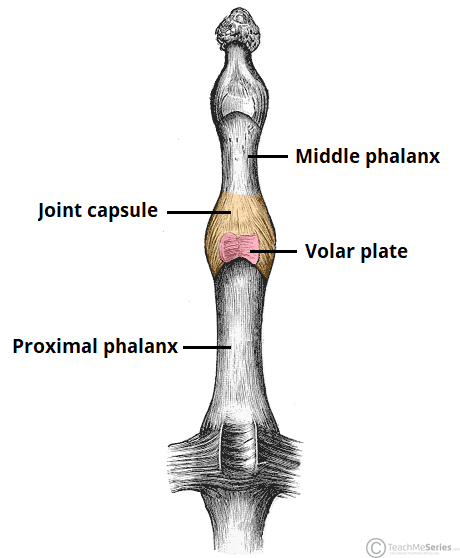
Fig 2 – Joint capsule and volar plate of the proximal interphalangeal joint (checkrein ligaments not shown on this illustration).
Ligaments
The proximal interphalangeal joint capsule is strengthened by surrounding ligaments:
- Proper and accessory collateral ligaments:
- The collateral ligaments are located on the radial and ulnar aspect of the joint. They prevent excessive adduction and abduction at the PIPJ.
- They arise from the head of the proximal phalanx and pass volarly onto the middle phalanx, along the lateral aspect of the joint.
- Each collateral ligament is accompanied by an accessory collateral ligament, originating from the same point, and extending anteriorly to attach to the volar plate.
- Volar plate:
- The volar plate is a thick fibrocartilaginous structure, which arches across the base of the PIPJ in a “U” shape. It prevents excessive hyperextension of the joint.
- It is attached to the head of the proximal phalanx via the checkrein ligaments and inserts distally onto the volar base of the middle phalanx.
Movements
Given the nature of hinge joints and the stability of the proximal interphalangeal joint, it only moves in one plane: flexion and extension.
- Flexion:
- A healthy PIPJ can flex to between 100-110°.
- The primary muscle that drives PIPJ flexion is flexor digitorum superficialis.
- The secondary driver of PIPJ flexion is flexor digitorum profundus (it primarily flexes the distal interphalangeal joint).
- Extension:
- Extension back to 0° is achieved by the extensor digitorum, lumbricals, and interossei muscle
- The index finger PIPJ gets further assistance from extensor indicis.
Clinical Relevance: Central Slip Tendon and Boutonnière Deformity
The muscles responsible for extension of the proximal interphalangeal joint form a complicated array of tendons and insertions along the finger.
The proximal interphalangeal joint is primarily extended by the central slip tendon, which inserts at the base of middle phalanx on the dorsal aspect.
Injury to the central slip can be caused by either trauma (e.g. laceration, blow to dorsal finger) or by inflammation (e.g. arthritis).
An untreated injury to the central slip tendon can result in a classical appearance known as the “Boutonnière deformity”. The PIPJ is unable to extend, and the DIPJ is hyperextended due to tension from the remaining extensor tendons.
Blood Supply
Arterial supply to the proximal interphalangeal joint is via the palmar digital arteries.
Innervation
Sensory innervation to the proximal interphalangeal joint is from the palmar digital nerves. They arise from branches of the median and ulnar nerves within the hand.
Clinical Relevance – Proximal Interphalangeal Joint Dislocation
Trauma to the hand can often result in dislocation of the proximal interphalangeal joint.
The PIPJ is most commonly dislocated in a dorsal direction, following a hyperextension-type mechanism of injury. It is often accompanied by a volar plate injury.
For most dislocations, the treatment consists of reduction (relocating the joint), and a period of splintage. Surgery repair of the ligaments may be required if the joint remains unstable.