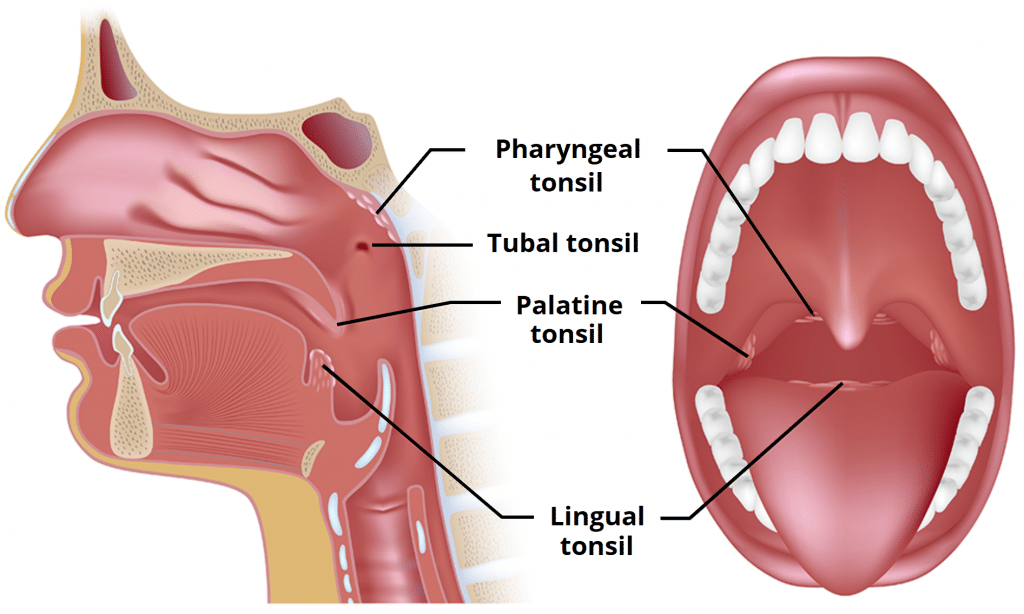
The tonsils are collections of lymphatic tissue located within the pharynx. They collectively form a ringed arrangement, known as Waldeyer’s ring:
- Pharyngeal tonsil
- Tubal tonsils (x2)
- Palatine tonsils (x2)
- Lingual tonsil
The tonsils are classified as mucosa-associated lymphoid tissue (MALT), and therefore contain T cells, B cells and macrophages. They have an important role in fighting infection – the first line of defence against pathogens entering through the nasopharynx or oropharynx.
In this article, we shall look at the anatomy of the tonsils – their location, blood supply and any clinical correlations.
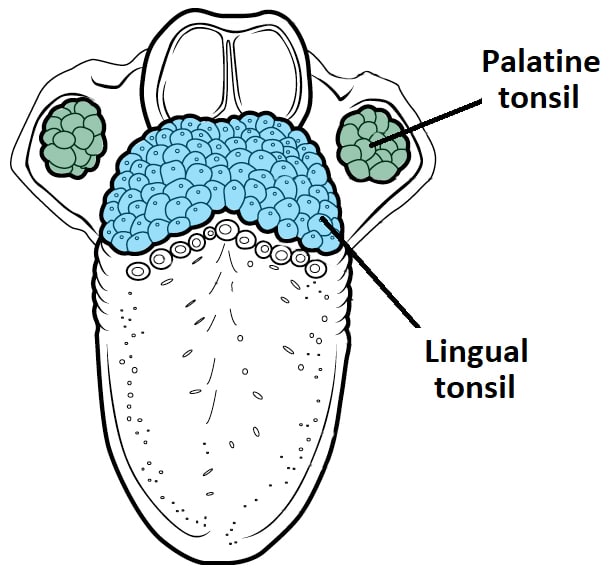
Lingual Tonsil
The lingual tonsil refers to numerous lymphoid nodules located within the submucosa of the posterior third of the tongue.
This tonsil is responsible for the irregular appearance of the posterior tongue surface. and forms the inferior part of Waldeyer’s ring.
Like the rest of the tongue, the lingual tonsil is covered by a stratified non-keratinised squamous epithelium.
Blood Supply and Innervation
The arterial supply to the lingual tonsil is largely via the lingual artery, with contributions from the tonsillar branch of the facial artery and the ascending pharyngeal artery.
The dorsal lingual branch of the lingual vein performs the venous drainage.
Innervation is from the glossopharyngeal nerve.
Lymphatic Drainage
Lymphatic fluid from the lingual tonsil drains into the jugulodigastric and deep cervical lymph nodes.
Pharyngeal Tonsil
The pharyngeal tonsil refers to a collection of lymphoid tissue within the mucosa of the roof of the nasopharynx. When enlarged, the pharyngeal tonsil is also known as the adenoids.
It is located in the midline of the nasopharynx, and forms the superior aspect of Waldeyer’s ring.
The epithelial covering of the pharyngeal tonsil is ciliated pseudostratified epithelium.
Blood Supply and Innervation
The pharyngeal tonsil receives arterial supply from several vessels:
- Ascending palatine artery
- Ascending pharyngeal artery (external carotid)
- Pharyngeal branch of the maxillary artery
- Artery of the pterygoid canal
- Basisphenoid artery
- Tonsillar branch of the facial artery
Venous drainage is via numerous small veins which pierce the superior constrictor muscle to empty into the pharyngeal plexus.
The pharyngeal tonsil receives nerve fibres from the vagus and glossopharyngeal cranial nerves.
Lymphatic Drainage
Lymphatic fluid from the pharyngeal tonsil drains into the retropharyngeal nodes (which empty into the deep cervical chain), and directly into deep cervical nodes within the parapharyngeal space.
Tubal Tonsils
The tubal tonsils refer to lymphoid tissue around the opening of the Eustachian tube in the lateral wall of the nasopharynx. They form the lateral aspect of the Waldeyer’s ring.
The epithelial covering of the tubal tonsils is ciliated pseudostratified epithelium.
Blood Supply and Innervation
The neurovascular supply is similar to other structures in the nasopharynx. Arterial supply is chiefly via the ascending pharyngeal artery and venous drainage is to the pharyngeal plexus.
Innervation is via the maxillary and glossopharyngeal nerves.
Lymphatic Drainage
The retropharyngeal and the deep cervical lymph nodes drain the tubal tonsils.
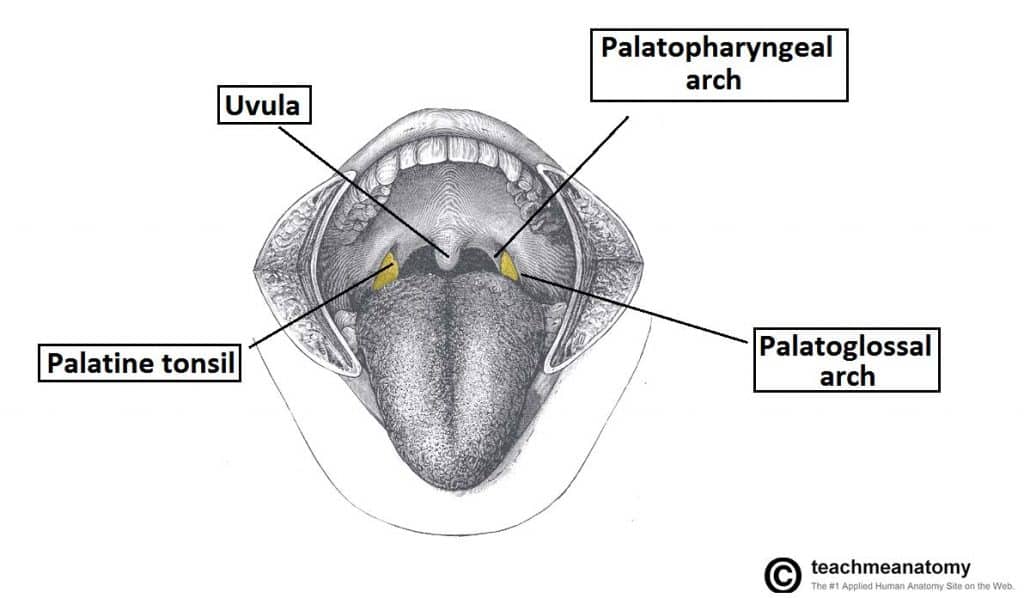
Palatine Tonsils
The palatine tonsils are commonly referred to as ‘the tonsils‘.
They are located within the tonsillar bed of the lateral oropharynx wall – between the palatoglossal arch (anteriorly) and palatopharyngeal arch (posteriorly). They form the lateral part of the Waldeyer’s ring.
Each tonsil has free medial surface which projects into the pharynx. The lateral surface is covered by a fibrous capsule, and is separated from the superior constrictor of the tonsillar bed by loose areolar connective tissue.
They are covered by a stratified non-keratinised squamous epithelium.
Blood Supply and Innervation
The arterial supply to the tonsil is via the tonsillar branch of the facial artery. It pierces the superior constrictor muscle to reach the palatine tonsil.
The venous drainage is via the external palatine vein (drains into the facial vein), and numerous smaller vessels which drain into the pharyngeal plexus.
The palatine tonsils receive innervation from the maxillary nerve and glossopharyngeal nerve.
Lymphatic Drainage
The palatine tonsils drain into the jugulodigastric and upper deep cervical lymph nodes.
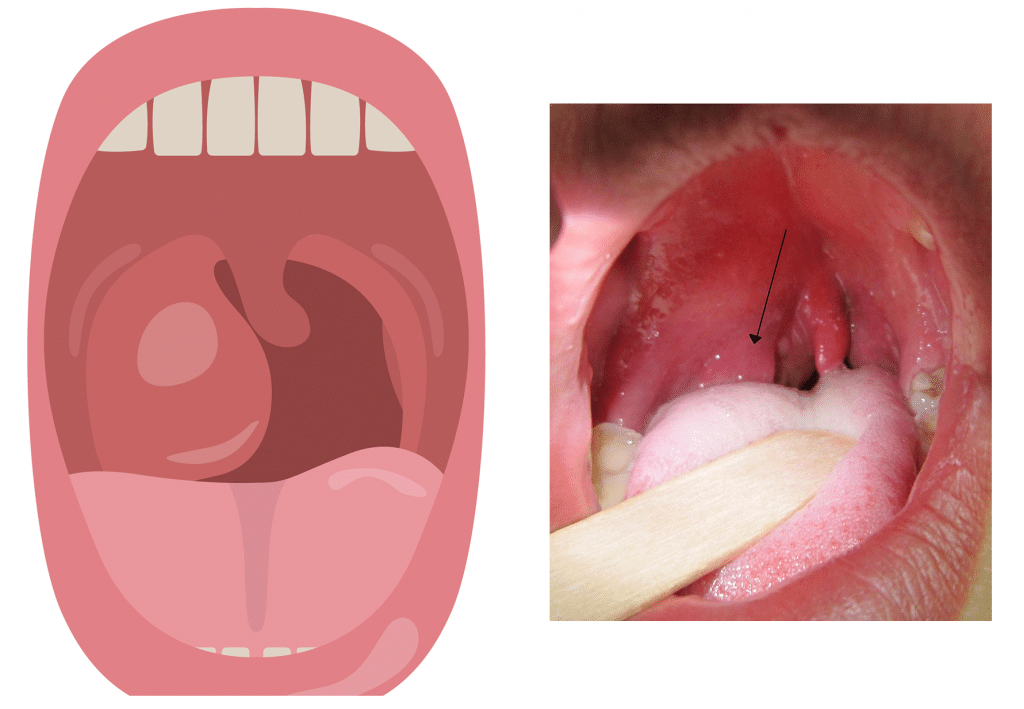
Clinical Relevance: Tonsillitis
Tonsillitis refers to inflammation of the palatine tonsils. It is usually caused by viral infection, with bacterial causes accounting for approximately 1/3 of cases.
Tonsillitis presents with difficult or painful swallowing – often with pyrexia and/or halitosis. On examination, the tonsils appear erythematous and swollen with evidence of purulent exudate and lymphadenopathy.
A complication of bacterial tonsillitis is a peritonsillar abscess (quinsy); a collection pus in the peritonsillar space. All quinsies will require drainage. There are two techniques adopted for this:
- Needle aspiration following topical local anaesthetic.
- Incision and drainage, with further opening via use of Magill forceps.