The testes and epididymis are paired structures, located within the scrotum. The testes are the site of sperm production and hormone synthesis, while the epididymis has a role in the storage of sperm.
In this article, we shall look at the anatomy of the testes and epididymis – their structure, vasculature, innervation and clinical correlations.
Anatomical Position
The testes are located within the scrotum, with the epididymis situated on the posterolateral aspect of each testicle. Commonly, the left testicle lies lower than the right. They are suspended from the abdomen by the spermatic cord – collection of vessels, nerves and ducts that supply the testes.
Originally, the testes are located on the posterior abdominal wall. During embryonic development they descend down the abdomen, and through the inguinal canal to reach the scrotum. They carry their neurovascular and lymphatic supply with them.
Anatomical Structure
The testes have an ellipsoid shape. They consist of a series of lobules, each containing seminiferous tubules supported by interstitial tissue. The seminiferous tubules are lined by Sertoli cells that aid the maturation process of the spermatozoa. In the interstitial tissue lie the Leydig cells that are responsible for testosterone production.
Spermatozoa are produced in the seminiferous tubules. The developing sperm travels through the tubules, collecting in the rete testes. Ducts known as efferent tubules transport the sperm from the rete testes to the epididymis for storage and maturation.
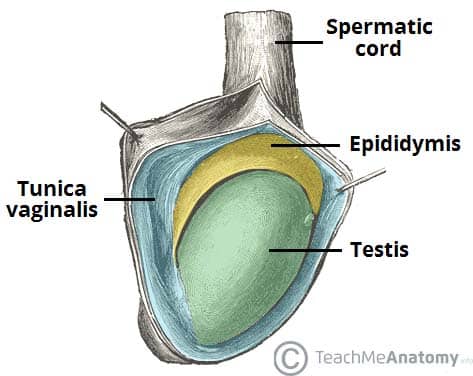
Inside the scrotum, the testes are covered almost entirely by the tunica vaginalis, a closed sac of parietal peritoneal origin that contains a small amount of viscous fluid. This sac covers the anterior surface and sides of each testicle and works much like the peritoneal sac, lubricating the surfaces of the testes and allowing for friction-free movement.
The testicular parenchyma is protected by the tunica albuginea, a fibrous capsule that encloses the testes. It penetrates into the parenchyma of each testicle with diaphragms, dividing it into lobules.
The epididymis consists of a single heavily coiled duct. It can be divided into three parts; head, body and tail.
- Head – The most proximal part of the epididymis. It is formed by the efferent tubules of the testes, which transport sperm from the testes to the epididymis.
- Body – Formed by the heavily coiled duct of the epididymis.
- Tail – The most distal part of the epididymis. It marks the origin of the vas deferens, which transports sperm to the prostatic portion of the urethra for ejaculation.
Innervation
The testes and epididymis receive innervation from the testicular plexus – a network of nerves derived from the renal and aortic plexi. They receive autonomic and sensory fibres.
Vascular Supply
The main arterial supply to the testes and epididymis is via the paired testicular arteries, which arise directly from the abdominal aorta. They descend down the abdomen, and pass into the scrotum via the inguinal canal, contained within the spermatic cord.
However, the testes are also supplied by branches of the cremasteric artery (from the inferior epigastric artery) and the artery of the vas deferens (from the inferior vesical artery). These branches give anastomoses to the main testicular artery.
Venous drainage is achieved via the paired testicular veins. They are formed from the pampiniform plexus in the scrotum – a network of veins wrapped around the testicular artery. In the retroperitoneal space of the abdomen, the left testicular vein drains into the left renal vein, while the right testicular vein drains directly into the inferior vena cava.
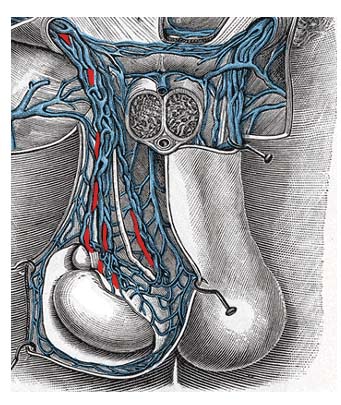
Fig 3 – The pampiniform plexus. Note how it surrounds the testicular artery.
Lymphatics
Since the testes are originally retroperitoneal organs, the lymphatic drainage is to the lumbar and para-aortic nodes, along the lumbar vertebrae.
This is in contrast to the scrotum, which drains into the nearby superficial inguinal nodes.
Clinical Relevance: Enlargement of the Scrotum
The scrotal sac is very distensible, and will enlarge in response to the size of its contents. There are a number of causes of scrotal swelling – here are the most common:
- Inguinal hernia – where the contents of the abdominal cavity protrude into the scrotum, via the inguinal canal.
- Hydrocoele – a collection of serous fluid within the tunica vaginalis. The congenital form is most commonly due to a failure of the processus vaginalis to close. Adult hydrocele is often associated with inflammation or trauma and rarely, testicular tumors.
- Haematocoele – a collection of blood in the tunica vaginalis. It can be distinguished from a hydrocoele by transillumination (where a light is applied to the testicular swelling). Due to the dense nature of blood, light is unable to pass through.
- Varicocoele – gross dilation of the veins draining the testes. The left testicle is more commonly affected, as the left testicular vein is longer and drains into the left renal vein at a perpendicular angle.
- A large varicocoele can look and feel like a “bag of worms” within the scrotum (Figure 4).
- Varicocoele is quite common in the general population; its prevalence is estimated at 15-25%.
- However this congenital situation should not be considered a disease – sperm quality is affected in only a small proportion of patients
- Epididymitis – inflammation of the epididymis, usually caused by bacterial or viral infection