The ulnar nerve is a major peripheral nerve of the upper limb.
In this article, we shall look at the anatomy of the ulnar nerve – its anatomical course, motor and sensory functions, and its clinical correlations.
Overview
- Spinal roots: C8-T1.
- Motor functions:
- Two muscles of the anterior forearm – flexor carpi ulnaris and medial half of flexor digitorum profundus
- Intrinsic muscles of the hand (apart from the thenar muscles and two lateral lumbricals)
- Sensory functions: Medial one and half fingers and the associated palm area.
Anatomical Course
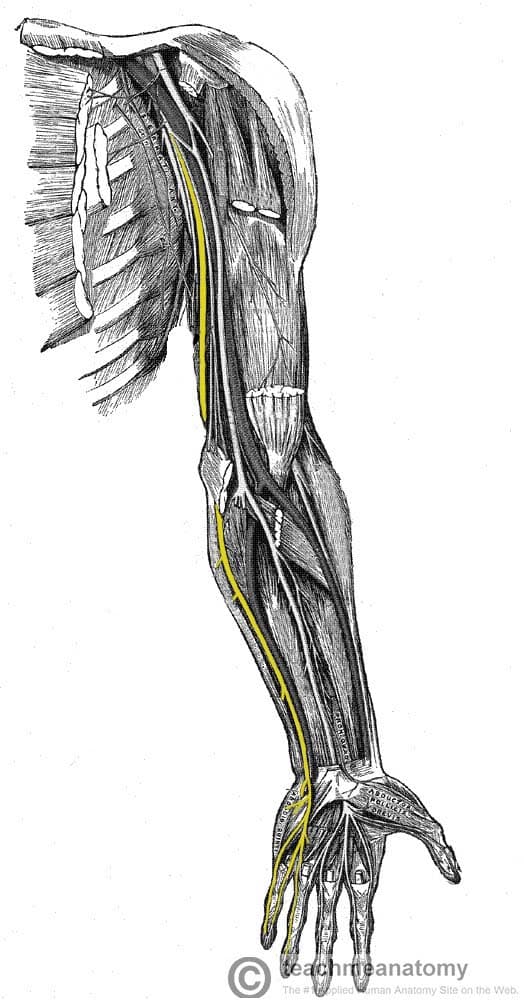
The ulnar nerve arises from the brachial plexus within the axilla region. It is a continuation of the medial cord and contains fibres from spinal roots C8 and T1.
After arising from the brachial plexus, the ulnar nerve descends in a plane between the axillary artery (lateral) and the axillary vein (medial). It proceeds down the medial aspect of the arm with the brachial artery located lateral.
At the mid-point of the arm, the ulnar nerve penetrates the medial fascial septum to enter the posterior compartment of the arm. It passes posterior to the elbow through the ulnar tunnel (small space between the medial epicondyle and olecranon). Here, it also gives arise to an articular branch which supplies the elbow joint.
In the forearm, the ulnar nerve pierces the two heads of the flexor carpi ulnaris, and travels deep to the muscle, alongside the ulna. Three main branches arise in the forearm:
- Muscular branch – innervates two muscles in the anterior compartment of the forearm.
- Palmar cutaneous branch – innervates the medial half of the palm.
- Dorsal cutaneous branch – innervates the dorsal surface of the medial one and a half fingers, and the associated dorsal hand area.
At the wrist, the ulnar nerve travels superficially to the flexor retinaculum, and is medial to the ulnar artery. It enters the hand via the ulnar canal (Guyon’s canal). In the hand, the nerve terminates by giving rise to superficial and deep branches.
Motor Functions
The ulnar nerve innervates muscles in the anterior compartment of the forearm, and in the hand.
Anterior Forearm
In the anterior forearm, the muscular branch of the ulnar nerve supplies two muscles:
- Flexor carpi ulnaris – flexes and adducts the hand at the wrist.
- Flexor digitorum profundus (medial half) – flexes the ring and little fingers at the distal interphalangeal joint
The remaining muscles in the anterior forearm are innervated by the median nerve.
Hand
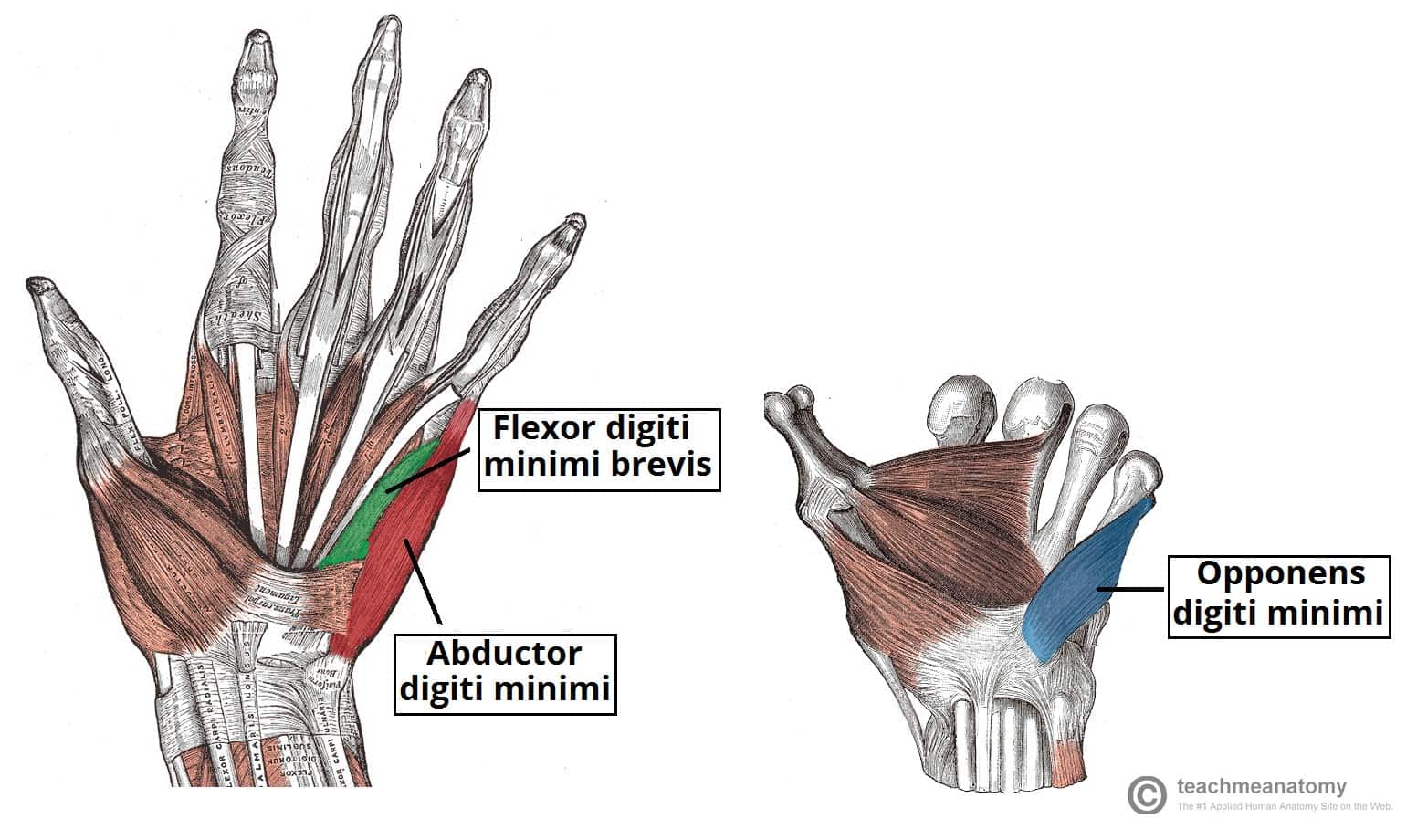
The majority of the intrinsic hand muscles are innervated by the deep branch of the ulnar nerve:
- Hypothenar muscles (flexor digiti minimi brevis, abductor digiti minimi, opponens digiti minimi)
- Medial two lumbricals
- Adductor pollicis
- Palmar and dorsal interossei of the hand
The palmaris brevis is an exception to this rule and is innervated by the superficial branch of the ulnar nerve. The other muscles of the hand (lateral two lumbricals and the thenar eminence) are innervated by the median nerve.
Clinical Relevance: Froment’s Sign
Froment’s sign is a test for ulnar nerve palsy – specifically paralysis of the adductor pollicis:
- The patient is asked to hold a piece of paper between the thumb and index finger, as the paper is pulled away.
- They should be able to hold the paper there with no difficulty (via adduction of the thumb).
- A positive test is when the patient is unable to adduct the thumb. Instead, they flex the thumb at the interphalangeal joint to try to maintain a hold on the paper.
Sensory Functions
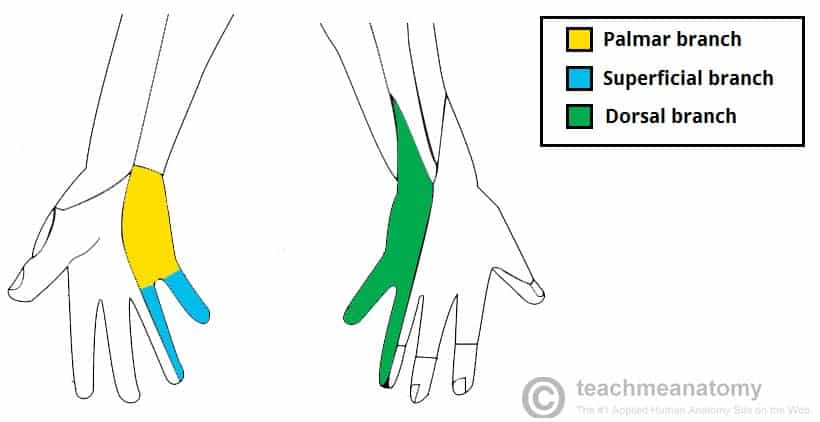
There are three branches of the ulnar nerve that are responsible for its sensory innervation.
Two of these branches arise in the forearm, and travel into the hand:
- Palmar cutaneous branch – innervates the medial half of the palm.
- Dorsal cutaneous branch – innervates the dorsal surface of the medial one and a half fingers, and the associated dorsal hand area.
The last branch arises in the hand itself:
- Superficial branch – innervates the palmar surface of the medial one and a half fingers.
Clinical Relevance: Ulnar Nerve Palsy
Damage at the Elbow
- Mechanism of injury: Trauma at the level of the medial epicondyle (e.g. isolated medial epicondyle fracture, supracondylar fracture). It can also be compressed in the cubital tunnel.
- Motor functions:
- All the muscles of innervated by the ulnar nerve are affected.
- Flexion of the wrist can still occur, but is accompanied by abduction (due to paralysis of flexor carpi ulnaris and medial half of flexor digitorum profundus).
- Abduction and adduction of the fingers cannot occur (due to paralysis of the interossei).
- Movement of the 4th and 5th digits is impaired (due to paralysis of the medial two lumbricals and hypothenar muscles).
- Adduction of the thumb is impaired, and the patient will have a positive Froment’s sign (due to paralysis of adductor pollicis).
- Sensory functions: All sensory branches are affected, so there will be a loss of sensation over the areas that the ulnar nerve innervates.
- Characteristic signs: Patient cannot grip paper placed between fingers, positive Froment’s sign, wasting of hypothenar eminence.
Damage at the Wrist
- Mechanism of injury: Lacerations to the anterior wrist.
- Motor functions:
- Only the intrinsic muscles of the hand are affected.
- Abduction and adduction of the fingers cannot occur (due to paralysis of the interossei).
- Movement of the 4th and 5th digits is impaired (due to paralysis of the medial two lumbricals and hypothenar muscles).
- Adduction of the thumb is impaired, and the patient will have a positive Froment’s sign (due to paralysis of adductor pollicis).
- Sensory functions: The palmar branch and superficial branch are usually severed, but the dorsal branch is unaffected. This results in sensory loss over palmar side of medial one and a half fingers only.
- Characteristic signs: Patient cannot grip paper placed between fingers, positive Froment’s sign, wasting of hypothenar eminence.