The median nerve is a major peripheral nerve of the upper limb.
In this article, we shall look at the anatomy of the median nerve – its anatomical course, motor and sensory functions, and clinical correlations.
Overview
- Nerve roots: C6 – T1 (also contains fibres from C5 in some individuals).
- Motor functions: Innervates the flexor and pronator muscles in the anterior compartment of the forearm (except the flexor carpi ulnaris and part of the flexor digitorum profundus, innervated by the ulnar nerve). Also supplies innervation to the thenar muscles and lateral two lumbricals in the hand.
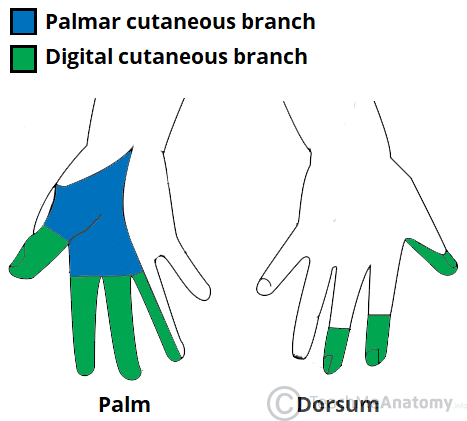
- Sensory functions: Gives rise to the palmar cutaneous branch, which innervates the lateral aspect of the palm, and the digital cutaneous branch, which innervates the lateral three and a half fingers on the anterior (palmar) surface of the hand.
Anatomical Course
The median nerve is derived from the medial and lateral cords of the brachial plexus. It contains fibres from roots C6-T1 and can contain fibres from C5 in some individuals.
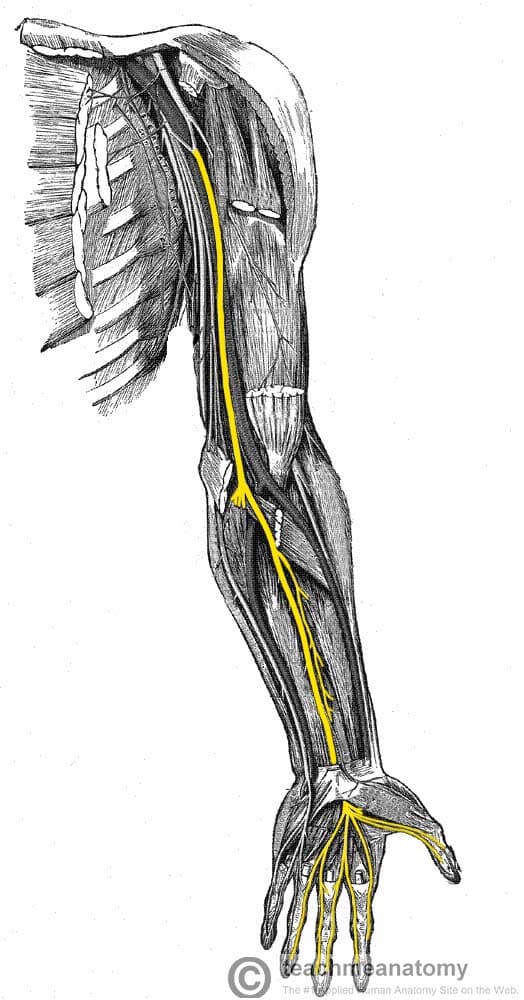
After originating from the brachial plexus in the axilla, the median nerve descends down the arm, initially lateral to the brachial artery. Halfway down the arm, the nerve crosses over the brachial artery, and becomes situated medially. The median nerve enters the anterior compartment of the forearm via the cubital fossa.
In the forearm, the nerve travels between the two heads of pronator teres, and then descends in a plane between the flexor digitorum profundus and flexor digitorum superficialis muscles. The median nerve gives rise to two major branches in the forearm:
- Anterior interosseous nerve – supplies the deep muscles in the anterior forearm.
- Palmar cutaneous nerve – innervates the skin of the lateral palm.
(The functions of these nerves are explored in more detail later in the article).
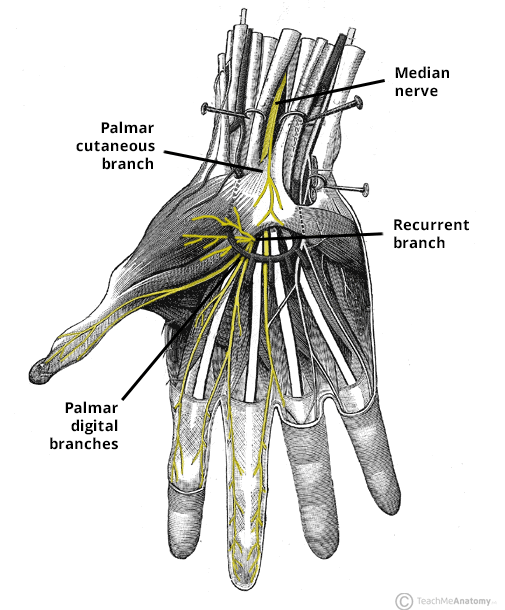
After giving off the anterior interosseous and palmar cutaneous branches, the median nerve enters the hand via the carpal tunnel – where it terminates by dividing into two branches:
- Recurrent branch – innervates the thenar muscles.
- Palmar digital nerves – innervate the palmar surface and fingertips of the lateral three and half digits. Also provides branches to the lateral two lumbrical muscles.
Clinical Relevance: Carpal Tunnel Syndrome
Compression of the median nerve within the carpal tunnel can cause carpal tunnel syndrome (CTS).
It is the most common mononeuropathy and is caused by an increased tissue pressure within the carpal tunnel. Whilst risk factors for CTS have been identified (such as diabetes, pregnancy and acromegaly), the exact underlying aetiology is not well understood.
Clinical features include numbness, tingling, and pain in the distribution of the median nerve. Importantly, the palm is usually spared – as the palmar cutaneous branch does not travel through the carpal tunnel. Symptoms can wake the patient from sleep and are usually worse in the morning. If left untreated, chronic CTS can cause weakness and atrophy of the thenar muscles.
Tests for carpal tunnel syndrome can be performed during physical examination:
- Tinel’s sign – tapping the nerve in the carpal tunnel to elicit pain in median nerve distribution.
- Phalen’s manoeuvre – holding the wrist in flexion for 60 seconds to elicit numbness/pain in median nerve distribution.
Treatment involves the use of a splint, holding the wrist in extension overnight to relieve symptoms. If this is unsuccessful, corticosteroid injections into the carpal tunnel can be trialled. Surgical decompression of the carpal tunnel may be required in severe cases.
Motor Functions
The median nerve innervates the majority of the muscles in the anterior forearm, and some intrinsic hand muscles.
Anterior Forearm
In the forearm, the median nerve directly innervates muscles in the superficial and intermediate layers:
- Superficial layer – pronator teres, flexor carpi radialis and palmaris longus.
- Intermediate layer – flexor digitorum superficialis.
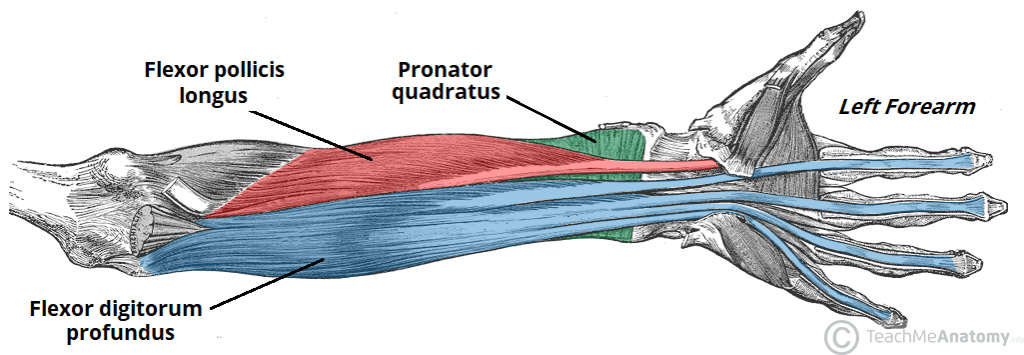
The median nerve also gives rise to the anterior interosseous nerve, which supplies the deep flexors:
- Deep layer – flexor pollicis longus, pronator quadratus, and the lateral half of the flexor digitorum profundus (the medial half of the muscle is innervated by the ulnar nerve).
In general, these muscles perform pronation of the forearm, flexion of the wrist and flexion of the digits of the hand.
Hand
The median nerve innervates some of the muscles in the hand via two branches.
The recurrent branch of the median nerve innervates the thenar muscles (muscles associated with movements of the thumb). The palmar digital branches innervates the lateral two lumbricals – these muscles perform flexion at the metacarpophalangeal joints and extension at the interphalangeal joints of the index and middle fingers
(The remaining muscles in the anterior forearm and hand are innervated by the ulnar nerve).
Sensory Functions
The median nerve is responsible for the cutaneous innervation of part of the hand. This is achieved via two branches:
- Palmar cutaneous branch – arises in the forearm and travels into the hand. It innervates the lateral aspect of the palm. This nerve does not pass through the carpal tunnel, and is spared in carpal tunnel syndrome.
- Palmar digital cutaneous branches – arise in the hand. Innervates the palmar surface and fingertips of the lateral three and half digits.
Clinical Relevance: Lesions of the Median Nerve
Damaged at the Elbow
- Mechanism of injury: Supracondylar fracture of the humerus.
- Motor functions: The flexors and pronators in the forearm are paralysed, with the exception of the flexor carpi ulnaris and medial half of flexor digitorum profundus. The forearm constantly supinated, and wrist flexion is weak (often accompanied by adduction, because of the pull of the flexor carpi ulnaris).
- Flexion at the thumb is also prevented, as both the longus and brevis muscles are paralysed.
- The lateral two lumbricals are affected, and the patient will not be able to flex at the MCP joints or extend at IP joints of the index and middle fingers.
- Sensory functions: Lack of sensation over the areas that the median nerve innervates.
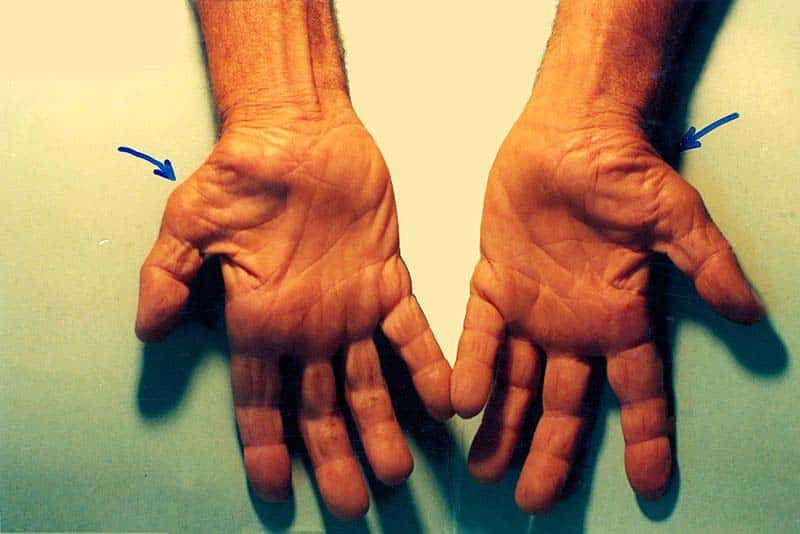
- Characteristic signs: The thenar eminence is wasted, due to atrophy of the thenar muscles. If patient tries to make a fist, only the little and ring fingers can flex completely. This results in a characteristic shape of the hand, known as hand of benediction.
Damaged at the Wrist
- Mechanism of injury: Lacerations just proximal to the flexor retinaculum.
- Motor functions: Thenar muscles paralysed, as are the lateral two lumbricals. This affects opposition of the thumb and flexion of the index and middle fingers.
- Sensory functions: Same as an injury at the elbow.
- Characteristic signs: The hand is held in the same position as damage at the elbow, but the forearm is unaffected (not supinated or adducted, wrist flexion likely unaffected, depending on the location of the lesion).