The axillary nerve is a major peripheral nerve of the upper limb.
In this article, we shall look at the anatomy of the axillary nerve – its anatomical course, motor and sensory functions, and any clinical correlations.
Overview
- Spinal roots: C5 and C6.
- Sensory functions: Gives rise to the upper lateral cutaneous nerve of arm, which innervates the skin over the lower deltoid (‘regimental badge area’).
- Motor functions: Innervates the teres minor and deltoid muscles.
Anatomical Course
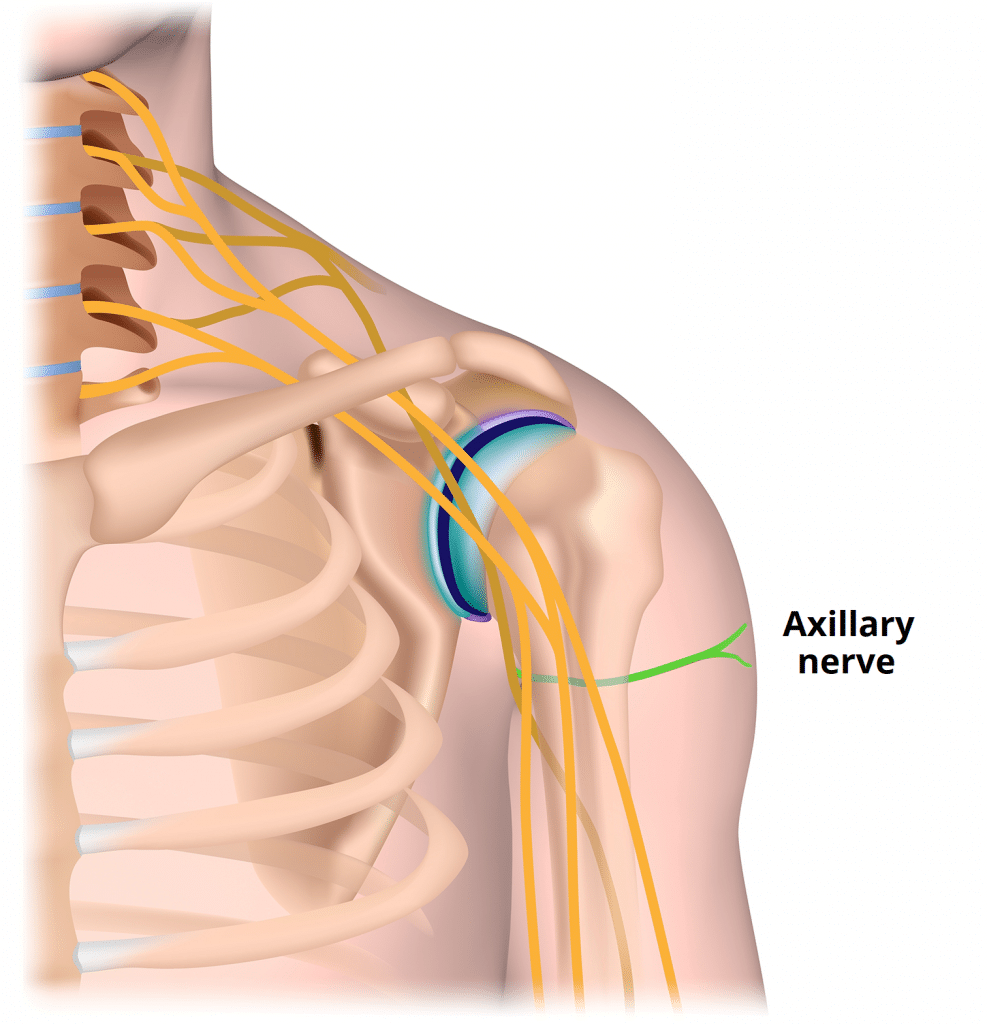
The axillary nerve is formed within the axilla area of the upper limb. It is a direct continuation of the posterior cord from the brachial plexus – and therefore contains fibres from the C5 and C6 nerve roots.
In the axilla, the axillary nerve is located posterior to the axillary artery and anterior to the subscapularis muscle. It exits the axilla at the inferior border of subscapularis via the quadrangular space, often accompanied by the posterior circumflex humeral artery and vein.
The axillary nerve then passes medially to the surgical neck of the humerus, where it divides into three terminal branches:
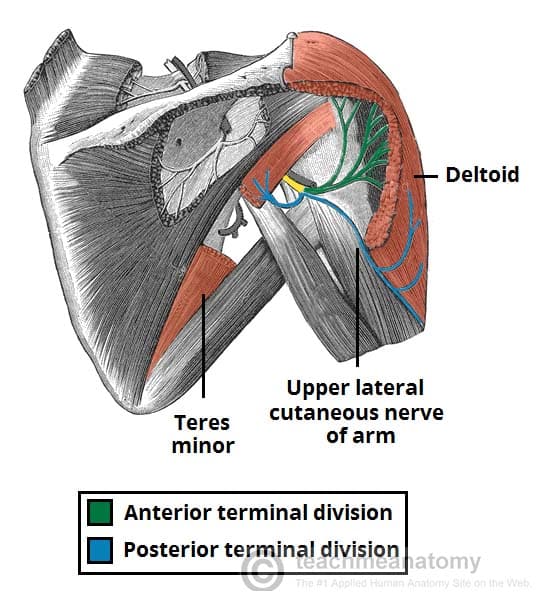
- Posterior terminal branch – provides motor innervation to the posterior aspect of the deltoid muscle and teres minor. It also innervates the skin over the inferior part of the deltoid as the upper lateral cutaneous nerve of the arm.
- Anterior terminal branch – winds around the surgical neck of the humerus and provides motor innervation to the anterior aspect of the deltoid muscle. It terminates with cutaneous branches to the anterior and anterolateral shoulder.
- Articular branch – supplies the glenohumeral joint
The Quadrangular Space
The quadrangular space is a gap in the muscles of the posterior scapular region. It is a pathway for neurovascular structures to move from the axilla anteriorly to the posterior shoulder and arm. It is bounded by:
- Superior – inferior aspect of teres minor
- Inferior – superior aspect of teres major
- Lateral – surgical neck of humerus.
- Medial – long head of triceps brachii
- Anterior – subscapularis
The axillary nerve and posterior circumflex humeral artery and vein pass through the quadrangular space. These structures can be compressed as a result of trauma, muscle hypertrophy or space occupying lesion; resulting in weakness of the deltoid and teres minor. This is particularly common in athletes who perform overhead activities.
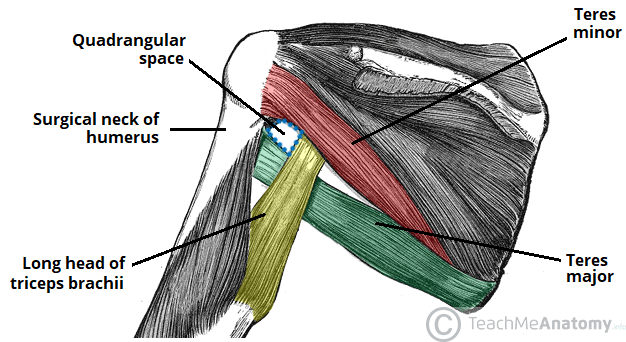
Fig 3 – Posterior view of the shoulder region, showing the quadrangular space. The subscapularis muscle lies anteriorly, and so cannot be seen.
Motor Functions
The axillary nerve innervates teres minor and deltoid muscles.
- Teres minor – part of the rotator cuff muscles which act to stabilise the glenohumeral joint. It acts to externally rotate the shoulder joint and is innervated by the posterior terminal branch of the axillary nerve.
- Deltoid – situated at the superior aspect of the shoulder. It performs abduction of the upper limb at the glenohumeral joint and is innervated by the anterior terminal branch of the axillary nerve.
NB: There is some evidence from research on cadavers that the axillary nerve can also innervate the lateral head of triceps brachii muscle.
Sensory Functions
The sensory component of the axillary nerve is delivered via its posterior terminal branch.
After the posterior terminal branch of the axillary nerve has innervated the teres minor, it continues as the upper lateral cutaneous nerve of the arm. It innervates the skin over the inferior portion of the deltoid (the ‘regimental badge area’).
In a patient with axillary nerve damage, sensation at the regimental badge area may be impaired or absent. The patient may also report paraesthesia (pins and needles) in the distribution of the axillary nerve.

Fig 4 – The sensory innervation of the axillary nerve – known as the regimental badge area.
Clinical Relevance: Injury to the Axillary Nerve
The axillary nerve can be damaged through trauma to the proximal humerus or shoulder girdle. It often presents with other brachial plexus injuries.
Common mechanisms of injury include fracture of the humeral surgical neck, shoulder dislocation or iatrogenic injury during shoulder surgery.
- Motor functions – the deltoid and teres minor muscles will be affected, rendering the patient unable to abduct the affected limb beyond 15 degrees.
- Sensory functions – the upper lateral cutaneous nerve of arm will be affected, resulting in loss of sensation over the inferior deltoid (‘regimental badge area’).
Clinical tests include deltoid extension lag and external rotation lag. Chronic lesions of the axillary nerve can result in permanent numbness at the lateral shoulder region, muscle atrophy, and neuropathic pain.
Clinical Relevance: Erb’s Palsy
Erb’s palsy is a condition resulting from damage to the C5 and C6 roots of the brachial plexus. The axillary nerve is therefore affected, and the individual is usually unable to abduct or externally rotate at the shoulder.
It commonly occurs where there is an excessive increase in the angle between the neck and shoulder, which stretches the nerve roots. The severity of the injury ranges from neuropraxia to avulsion, which determines recovery.