The brachial plexus is a network of nerve fibres that supplies the skin and musculature of the upper limb. It begins in the root of the neck, passes through the axilla, and runs through the entire upper extremity.
The plexus is formed by the anterior rami (divisions) of cervical spinal nerves C5, C6, C7 and C8, and the first thoracic spinal nerve, T1.
In this article, we shall look at the anatomy of the brachial plexus – its formation and anatomical course through the body.
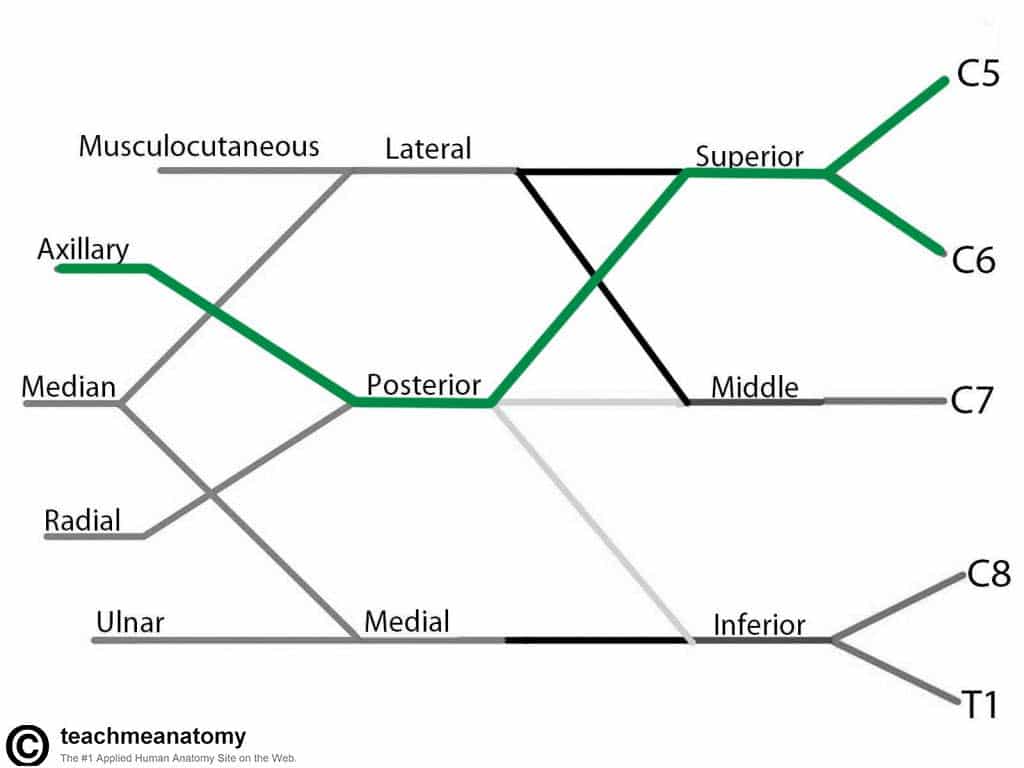
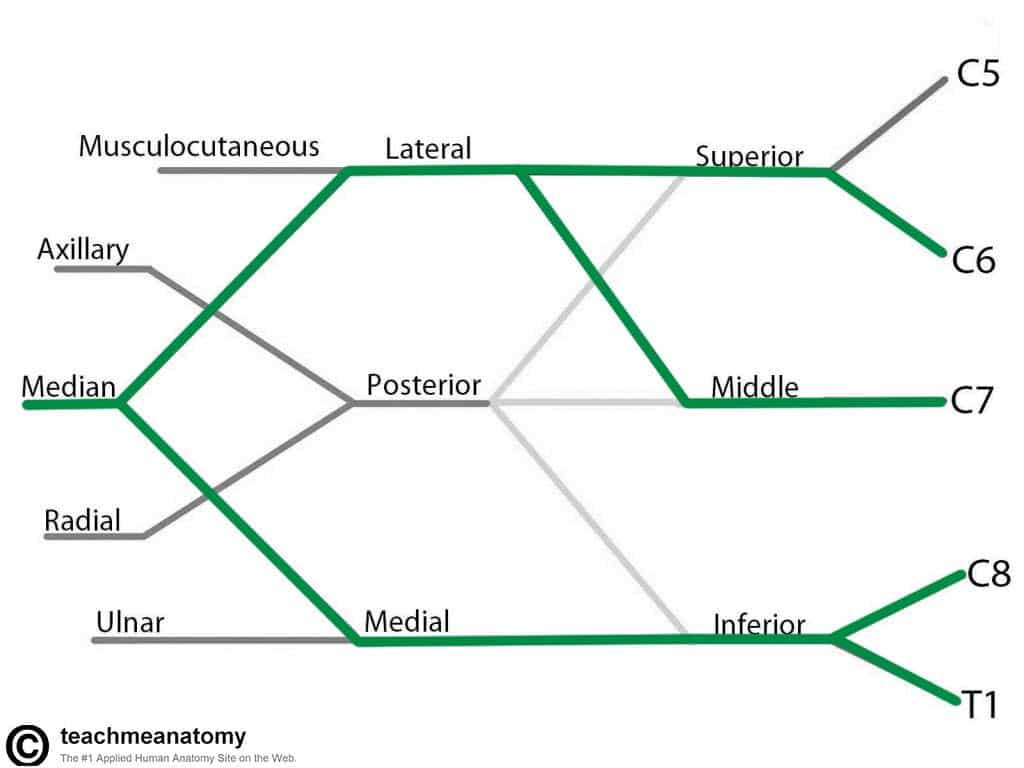
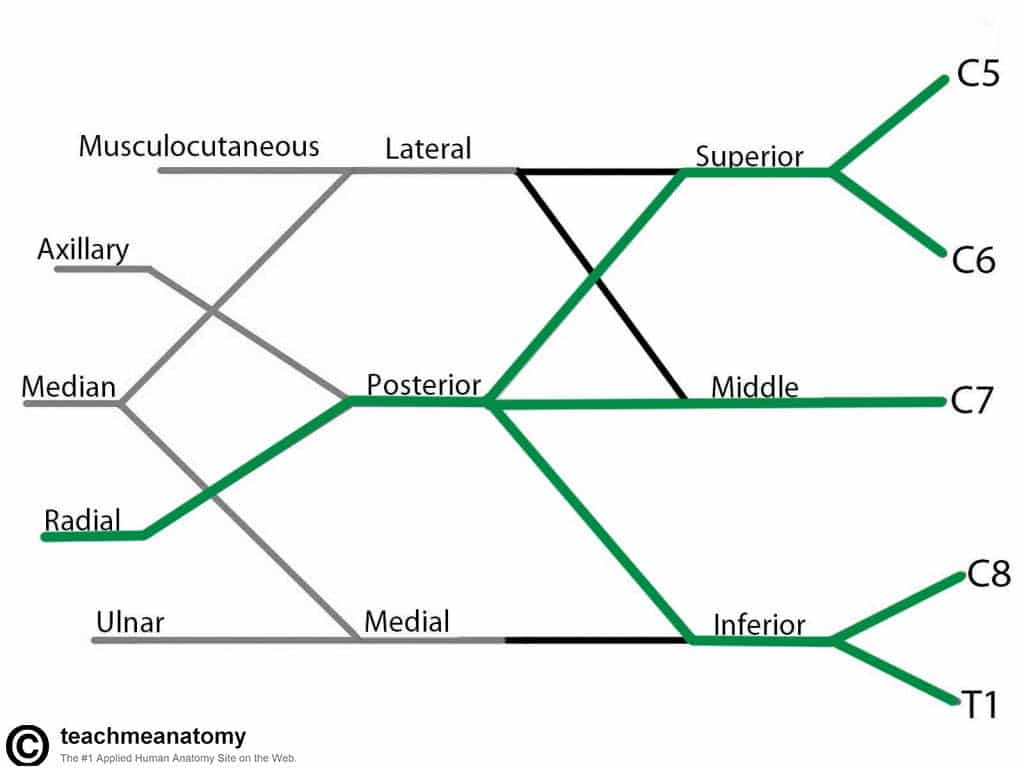
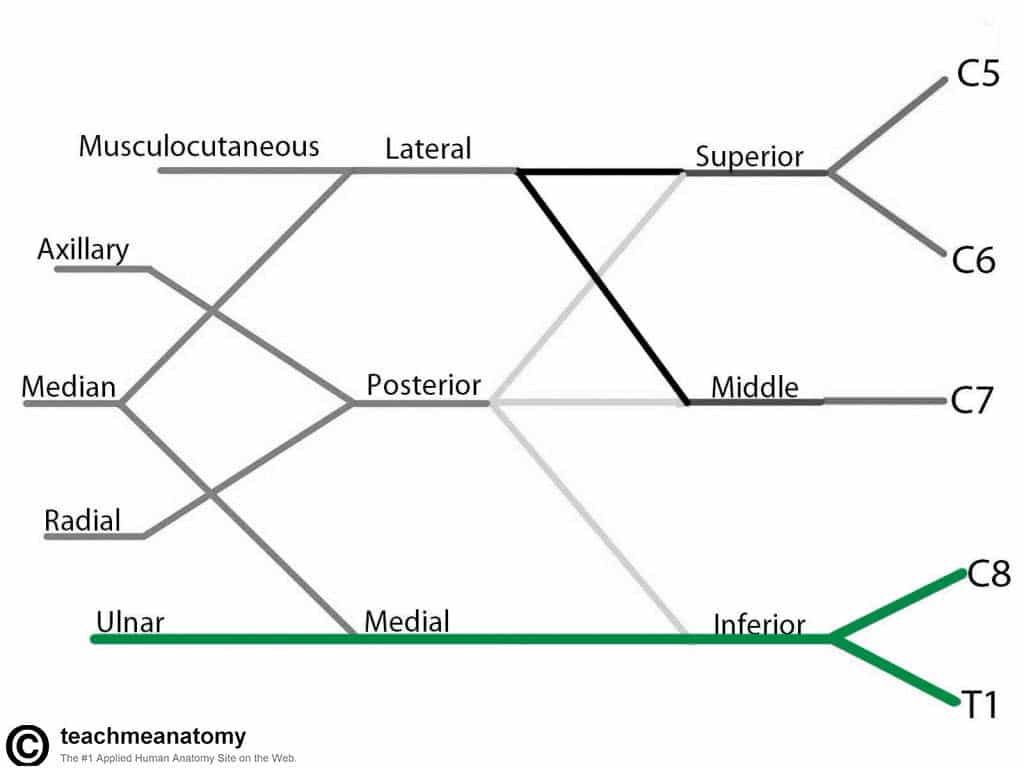
The brachial plexus is divided into five parts; roots, trunks, divisions, cords and branches (a good mnemonic for this is Read That Damn Cadaver Book). There are no functional differences between these divisions – they are simply used to aid explanation of the brachial plexus.
Roots
The ‘roots’ refer the anterior rami of the spinal nerves that comprise the brachial plexus. These are the anterior rami of spinal nerves C5, C6, C7, C8, and T1.
At each vertebral level, paired spinal nerves arise. They leave the spinal cord via the intervertebral foramina of the vertebral column.
Each spinal nerve then divides into an anterior and a posterior ramus. The roots of the brachial plexus are formed by the anterior rami of spinal nerves C5-T1 (the posterior divisions innervate the skin and musculature of the intrinsic back muscles).
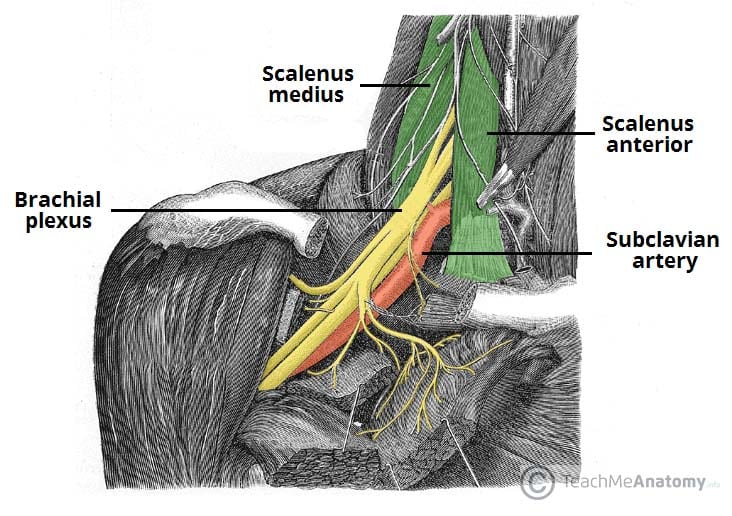
After their formation, these nerves pass between the anterior and medial scalene muscles to enter the base of the neck.
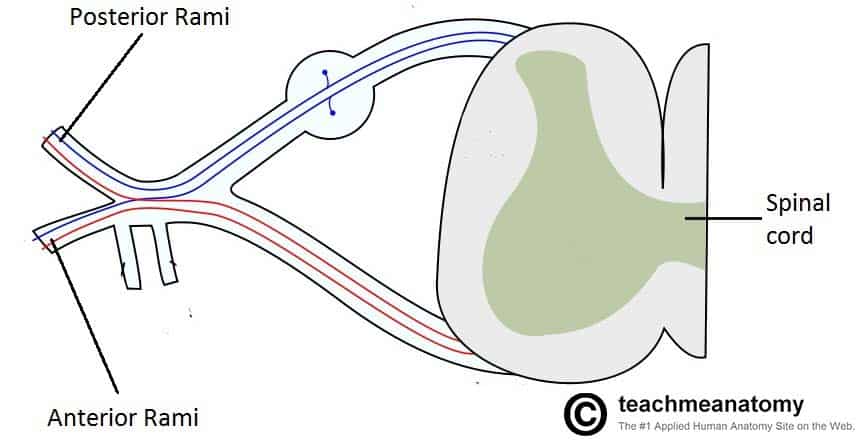
Fig 2 – The spinal cord outflow at each vertebral level. The anterior rami of vertebral levels C5-C8 and T1 make up the roots of the brachial plexus.
Trunks
At the base of the neck, the roots of the brachial plexus converge to form three trunks. These structures are named by their relative anatomical location:
- Superior trunk – a combination of C5 and C6 roots.
- Middle trunk – continuation of C7.
- Inferior trunk – combination of C8 and T1 roots.
The trunks traverse laterally, crossing the posterior triangle of the neck.
Divisions
Each trunk divides into two branches within the posterior triangle of the neck. One division moves anteriorly (toward the front of the body) and the other posteriorly (towards the back of the body). Thus, they are known as the anterior and posterior divisions.
We now have three anterior and three posterior nerve fibres. These divisions leave the posterior triangle and pass into the axilla. They recombine into the cords of the brachial plexus.
Cords
Once the anterior and posterior divisions have entered the axilla, they combine together to form three cords, named by their position relative to the axillary artery.
The lateral cord is formed by:
- The anterior division of the superior trunk
- The anterior division of the middle trunk
The posterior cord is formed by:
- The posterior division of the superior trunk
- The posterior division of the middle trunk
- The posterior division of the inferior trunk
The medial cord is formed by:
- The anterior division of the inferior trunk.
The cords give rise to the major branches of the brachial plexus.
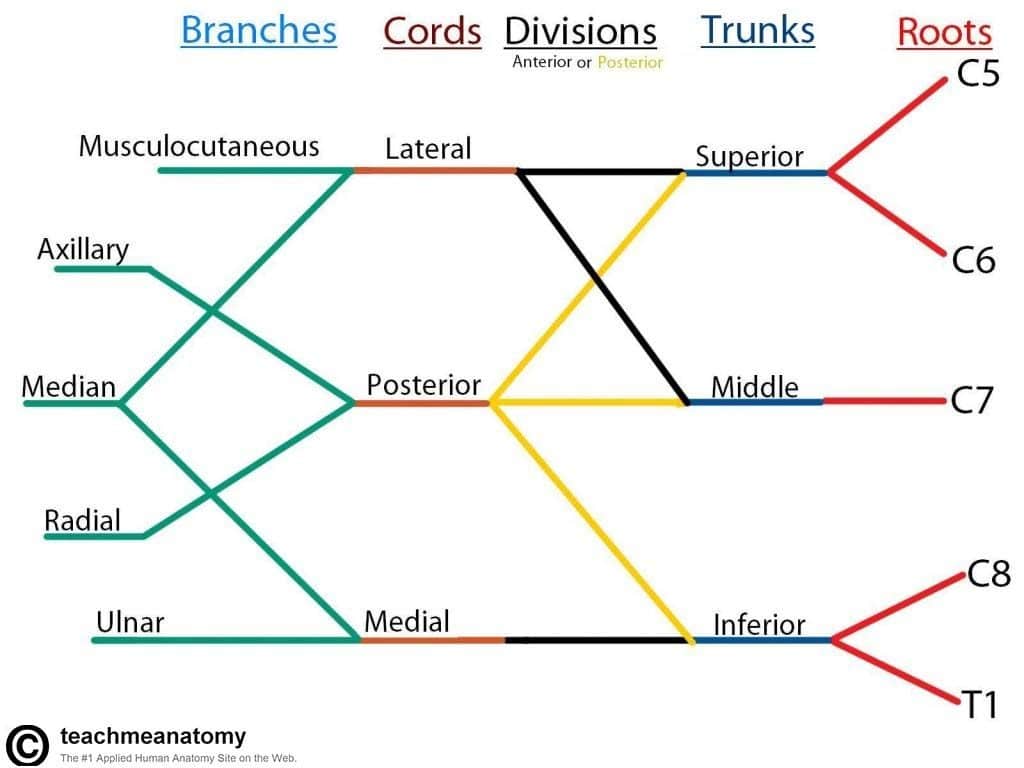
Fig 3 – Diagrammatic representation of the brachial plexus. For simplicity, the smaller branches of the brachial plexus are not shown. The posterior divisions are shown in yellow, and anterior divisions in black.
Major Branches
In the axilla and the proximal aspect of the upper limb, the three cords give rise to five major branches. These nerves continue into the upper limb to provide innervation to the muscles and skin present. In this section, we shall concentrate on these five nerves.
Note: these are only brief notes on the function of the nerves – for more detailed information click on the title to visit their respective pages.
Musculocutaneous Nerve
See more detailed information here.
- Roots: C5, C6, C7.
- Motor Functions: Innervates the brachialis, biceps brachii and coracobrachialis muscles.
- Sensory Functions: Gives off the lateral cutaneous branch of the forearm, which innervates the lateral half of the anterior forearm, and a small lateral portion of the posterior forearm.
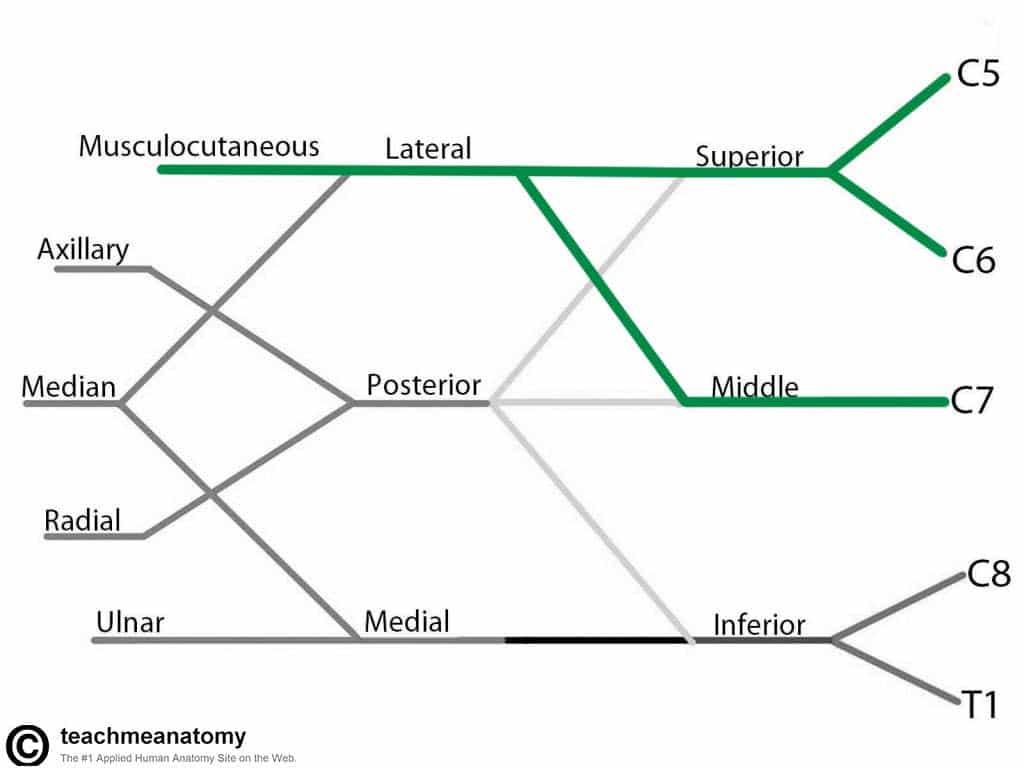
Fig 4 – The derivation of the musculocutaneous nerve from the brachial plexus
Axillary Nerve
See more detailed information here.
- Roots: C5 and C6.
- Motor Functions: Innervates the teres minor and deltoid muscles.
- Sensory Functions: Gives off the superior lateral cutaneous nerve of arm, which innervates the inferior region of the deltoid (“regimental badge area”).
Median Nerve
See more detailed information here.
- Roots: C6 – T1. (Also contains fibres from C5 in some individuals).
- Motor Functions: Innervates most of the flexor muscles in the forearm, the thenar muscles, and the two lateral lumbricals associated with the index and middle fingers.
- Sensory Functions: Gives off the palmar cutaneous branch, which innervates the lateral part of the palm, and the digital cutaneous branch, which innervates the lateral three and a half fingers on the anterior (palmar) surface of the hand.
Radial Nerve
See more detailed information here.
- Roots: C5 – T1.
- Motor Functions: Innervates the triceps brachii, and the muscles in the posterior compartment of the forearm (which are primarily, but not exclusively, extensors of the wrist and fingers).
- Sensory Functions: Innervates the posterior aspect of the arm and forearm, and the posterolateral aspect of the hand.
Ulnar Nerve
See more detailed information here
- Roots: C8 and T1.
- Motor Functions: Innervates the muscles of the hand (apart from the thenar muscles and two lateral lumbricals), flexor carpi ulnaris and medial half of flexor digitorum profundus.
- Sensory Functions: Innervates the anterior and posterior surfaces of the medial one and half fingers, and associated palm area.
Practical Relevance: Dissecting the Brachial Plexus
When dissecting the upper limb, it can be difficult to recognise what part of the brachial plexus you are at – it can just look like a mass of nerves.
The important structure to look for is an ‘M’ shape. This is formed by the musculocutaneous, median, and ulnar nerves, usually superficial to the axillary artery.
This shape is usually consistent between cadavers. It can help you get your bearings, and you can work backwards to identify the cords, divisions and branches.
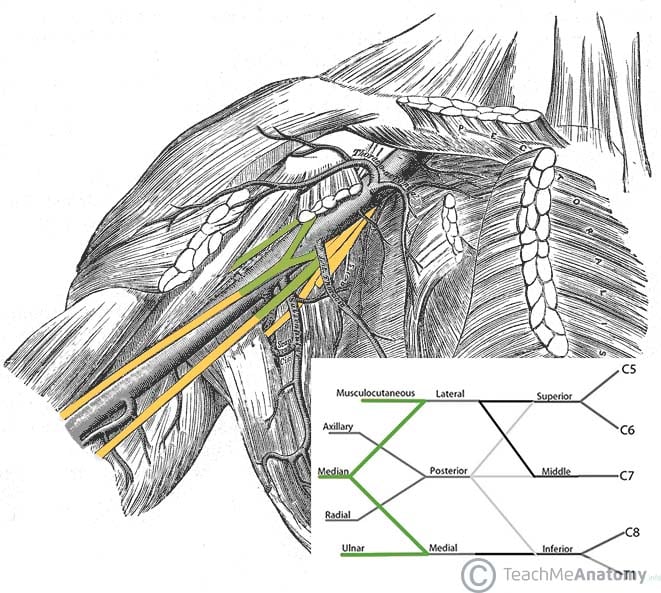
Fig 9 – The ‘M’ shape, consisting of the ulnar, median and musculocutaneous nerves.
Minor Branches
In addition to the five major branches of the brachial plexus, there are a number of smaller nerves that arise. They do so from all five parts of the brachial plexus, and are listed below:
| Roots | Trunks | Lateral cord | Medial cord | Posterior cord |
| Dorsal scapular nerve
Long thoracic nerve
|
Suprascapular nerve
Nerve to subclavius
|
Lateral pectoral nerve
|
Medial pectoral nerve
Medial cutaneous nerve of arm
Medial cutaneous nerve of forearm |
Superior subscapular nerve
Thoracodorsal nerve
Inferior subscapular nerve |
Clinical Relevance: Upper Brachial Plexus Injury (Erb’s Palsy)
Erb’s palsy refers to an injury to the upper roots of the brachial plexus (typically C5-6). It most commonly occurs as a result of a stretching injury during a difficult vaginal delivery.
- Nerves affected – the peripheral nerves derived from C5-6 roots are most affected. This includes the musculocutaneous, axillary, suprascapular, and nerve to subclavius.
- Muscles affected – supraspinatus, infraspinatus, subclavius, biceps brachii, brachialis, coracobrachialis, deltoid and teres minor.
- Motor functions affected – abduction at shoulder, lateral rotation of arm, supination of forearm, and flexion at shoulder.
- Sensory functions affected – sensation over the lateral aspect of upper limb (C5-6 dermatomes).
The affected limb hangs limply, medially rotated by the unopposed action of pectoralis major. The forearm is pronated due to the loss of biceps brachii. The wrist is weakly flexed due to the normal tone of the wrist flexors relative to the weakened wrist extensors. This is position is known as ‘waiter’s tip’ and is characteristic of Erb’s palsy.
Clinical Relevance: Lower Brachial Plexus Injury (Klumpke’s Palsy)
Klumpke’s palsy is an injury of the lower roots of the brachial plexus (C8-T1). It is also most commonly associated with a difficult vaginal delivery but has a much lower incidence than Erb’s palsy.
- Nerves affected – the peripheral nerves derived from T1 root are most affected; the ulnar and median nerves
- Muscles affected – the intrinsic hand muscles
- Sensory functions affected – sensation along medial side of upper limb (C8-T1 dermatomes).
The primary feature of Klumpke’s palsy is a clawed hand. This occurs due to paralysis of the lumbrical muscles, which normally act to flex the metacarpophalangeal joints (MCPJs) and extend the interphalangeal joints (IPJs). When paralysed, the fingers subsequently become extended at the MCPJs and flexed at the IPJs, producing a clawed appearance.