The shoulder joint (glenohumeral joint) is an articulation between the scapula and the humerus.
It is a ball and socket-type synovial joint, and one of the most mobile joints in the human body.
In this article, we shall look at the anatomy of the shoulder joint – its structure, blood supply, and clinical correlations.
Anatomical Structure
Articulating Surfaces
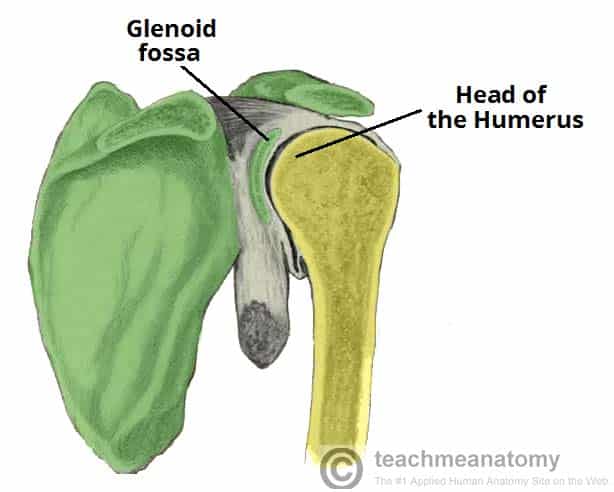
The shoulder joint is formed by an articulation between the head of the humerus and the glenoid cavity (or fossa) of the scapula. This gives rise to the alternate name for the shoulder joint – the glenohumeral joint.
Like most synovial joints, the articulating surfaces are covered with hyaline cartilage.
The head of the humerus is much larger than the glenoid fossa, giving the joint a wide range of movement at the cost of instability. To reduce the disproportion in surfaces, the glenoid fossa is deepened by a fibrocartilage rim – called the glenoid labrum.
Joint Capsule
The joint capsule is a fibrous sheath which encloses the structures of the joint.
It extends from the anatomical neck of the humerus to the border or ‘rim’ of the glenoid fossa. The joint capsule is lax – permitting greater mobility (particularly abduction).
The synovial membrane lines the inner surface of the joint capsule and produces synovial fluid to reduce friction between the articular surfaces.
Ligaments
Ligaments play an important role in stabilising the shoulder joint:
- Glenohumeral ligaments (superior, middle and inferior) – extend from the humerus to the glenoid fossa, reinforcing the joint capsule. They act to stabilise the anterior aspect of the joint.
- Coracohumeral ligament – extends from the base of the coracoid process to the greater tubercle of the humerus. It supports the superior part of the joint capsule.
- Transverse humeral ligament – extends between the two tubercles of the humerus. It holds the tendon of the long head of the biceps in the intertubercular groove.
- Coracoacromial ligament – extends between the acromion and coracoid process of the scapula, forming an arch-like structure over the shoulder joint (coracoacromial arch). This resists superior displacement of the humeral head.
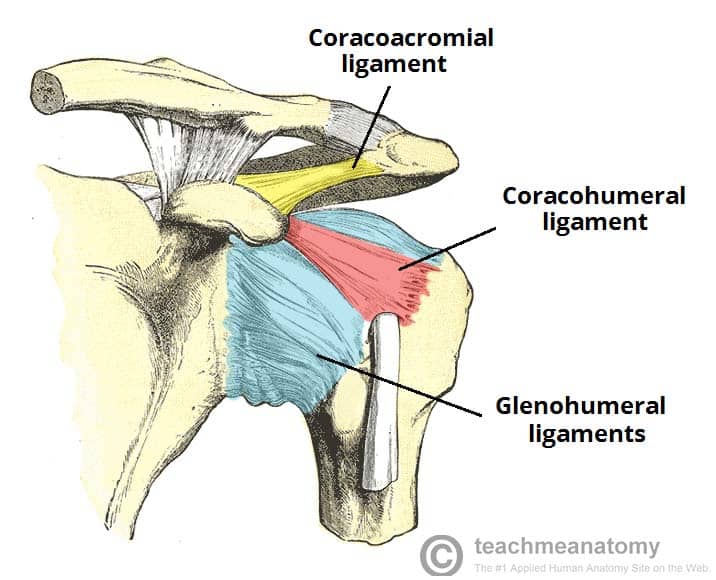
Fig 2 – The ligaments of the shoulder joint. The transverse humeral ligament is not shown on this diagram
Bursae
A bursa is a sac-like structure containing a small amount of synovial fluid. It functions to decrease friction between tendons, bone, and skin during movement. There are several bursae present in the shoulder joint:
- Subacromial – located deep to the deltoid and acromion, and superficial to the supraspinatus tendon and joint capsule.
- It reduces friction beneath the deltoid, promoting free motion of the rotator cuff tendons.
- Subscapular – located between the subscapularis tendon and the scapula.
- It reduces friction on the tendon during movement at the shoulder joint.
There are other minor bursae present between the tendons of the muscles around the joint.
Movements
The shoulder joint is an extremely mobile joint, with a wide range of movement possible:
- Extension (upper limb backwards in sagittal plane) – posterior deltoid, latissimus dorsi and teres major.
- Flexion (upper limb forwards in sagittal plane) – pectoralis major, anterior deltoid and coracobrachialis. Biceps brachii weakly assists in forward flexion.
- Abduction (upper limb away from midline in coronal plane):
- The first 0-15 degrees of abduction is produced by the supraspinatus.
- The middle fibres of the deltoid are responsible for the next 15-90 degrees.
- Past 90 degrees, the scapula needs to be rotated to achieve abduction – that is carried out by the trapezius and serratus anterior.
- Adduction (upper limb towards midline in coronal plane) – pectoralis major, latissimus dorsi and teres major.
- Internal rotation (rotation towards the midline, so that the thumb is pointing medially) – subscapularis, pectoralis major, latissimus dorsi, teres major and anterior deltoid.
- External rotation (rotation away from the midline, so that the thumb is pointing laterally) – infraspinatus and teres minor.
- Circumduction (moving the upper limb in a circle) – produced by a combination of the movements described above.
Mobility and Stability
The shoulder joint is one of the most mobile in the body, at the expense of stability. Here, we shall consider the factors the permit movement, and those that contribute towards joint structure.
Mobility:
- Type of joint – ball and socket joint.
- Bony surfaces – shallow glenoid cavity and large humeral head – there is a 1:4 disproportion in surfaces. A commonly used analogy is the golf ball and tee.
- Joint capsule – lax
Stability:
- Rotator cuff muscles – surround the shoulder joint, attaching to the tuberosities of the humerus, whilst also fusing with the joint capsule. The resting tone of these muscles act to compress the humeral head into the glenoid cavity.
- Glenoid labrum – a fibrocartilaginous ridge surrounding the glenoid cavity. It deepens the cavity and creates a seal with the head of humerus, reducing the risk of dislocation.
- Ligaments – act to reinforce the joint capsule and form the coracoacromial arch.
- Biceps tendon – it acts as a minor humeral head depressor, thereby contributing to stability.
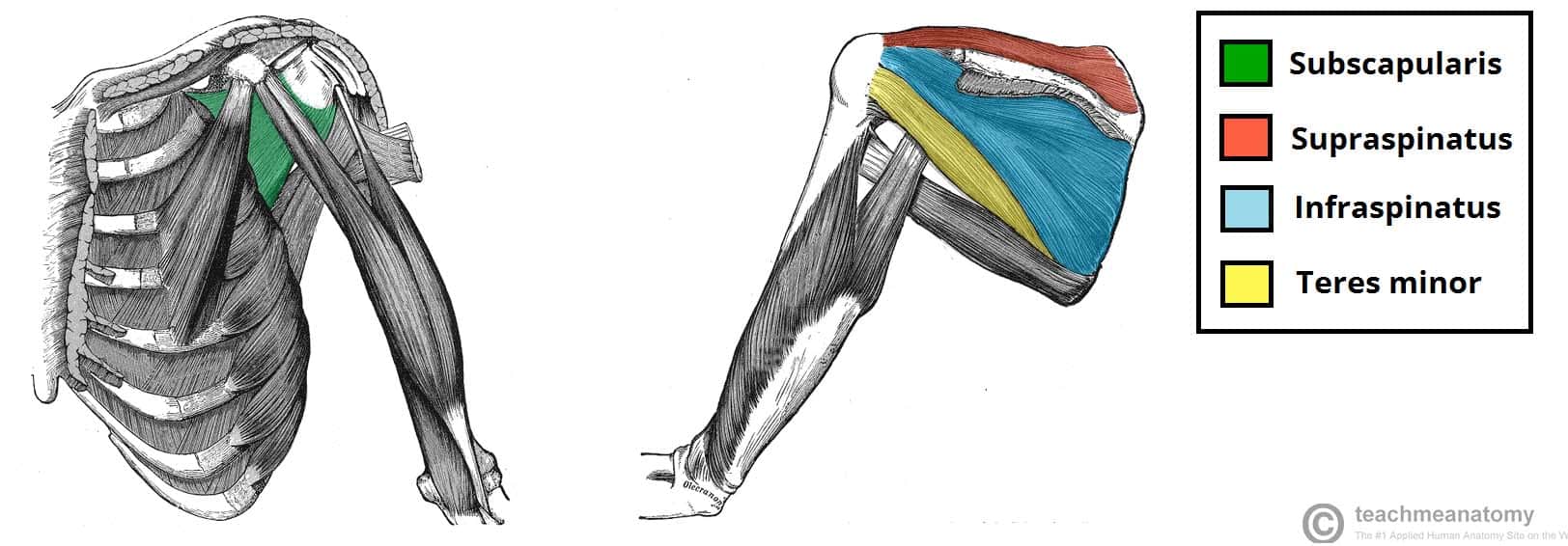
Fig 4 – The rotator cuff muscles, which act to stabilise the shoulder joint.
Blood Supply
The shoulder joint is supplied by the anterior and posterior circumflex humeral arteries – which are both branches of the axillary artery.
There are also contributions from the suprascapular artery (itself a branch of the thyrocervical trunk).
Innervation
Sensory innervation to the shoulder joint is from the axillary and suprascapular nerves.
Clinical Relevance: Common Injuries
Dislocation of the Shoulder Joint
Clinically, dislocations at the shoulder are described by where the humeral head lies in relation to the glenoid fossa. Anterior dislocations are the most prevalent (95%), although posterior (4%) and inferior (1%) dislocations can sometimes occur. Superior displacement of the humeral head is generally prevented by the coraco-acromial arch.
An anterior dislocation is usually caused by excessive extension and lateral rotation of the humerus. The humeral head is forced anteriorly and inferiorly – into the weakest part of the joint capsule. Tearing of the joint capsule is associated with an increased risk of future dislocations. Hill-Sachs lesions (impaction fracture of posterolateral humeral head against anteroinferior glenoid) and Bankart lesions (detachment of antero-inferior labrum with or without an avulsion fracture) can also occur following anterior dislocation.
Indeed, so-called ‘reverse Hill-Sachs lesions’ (impaction fracture of anteromedial humeral head) and ‘reverse Bankart lesions’ (detachment of posteroinferior labrum) can be seen in posterior dislocations.
The axillary nerve runs in close proximity to the shoulder joint and around the surgical neck of the humerus, and so it can be damaged in the dislocation or with attempted reduction. Injury to the axillary nerve causes paralysis of the deltoid, and loss of sensation over regimental badge area.
Rotator Cuff Tendonitis
The rotator cuff muscles have a very important role in stabilising the glenohumeral joint. They are often under heavy strain, and therefore injuries of these muscles are relatively common.
The spectrum of rotator cuff pathology comprises tendinitis, shoulder impingement and sub-acromial bursitis. Tendinitis refers to inflammation of the muscle tendons – usually due to overuse. Over time, this causes degenerative changes in the subacromial bursa and the supraspinatus tendon, potentially causing bursitis and impingement.
The characteristic sign of supraspinatus tendinitis is the ‘painful arc’ – pain in the middle of abduction between 60-120 degrees, where the affected area comes into contact with the acromion. This sign may also suggest a partial tear of supraspinatus.