The urethra is the vessel responsible for transporting urine from the bladder to an external opening in the perineum.
It is lined by stratified columnar epithelium, which is protected from the corrosive urine by mucus secreting glands.
In this article, we shall look at the anatomy of the male and female urethra – their anatomical course, neurovascular supply, and any clinical correlations.
Male Urethra
The male urethra is approximately 15-20cm long. In addition to urine, the male urethra transports semen – a fluid containing spermatozoa and sex gland secretions.
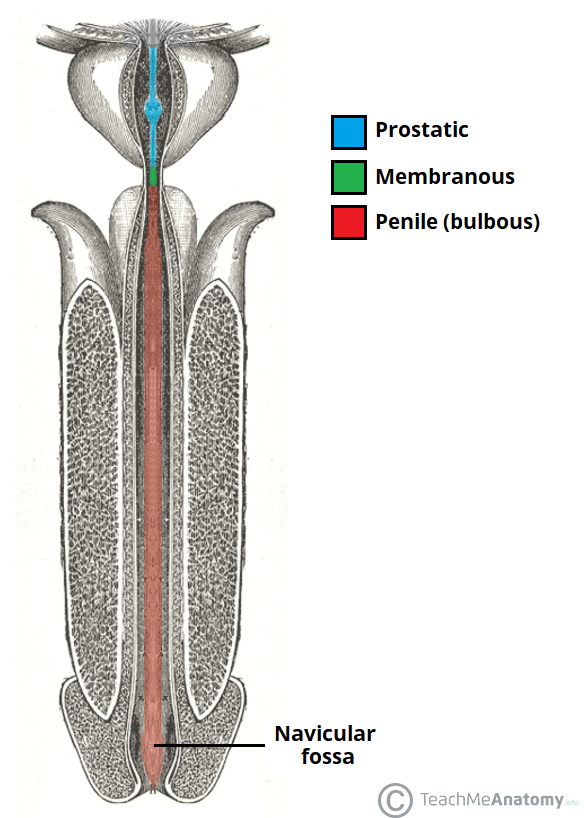
Fig 1 – Coronal section of the penis, showing the three parts of the urethra.
According to the latest classification, the male urethra can be divided anatomically into three parts (proximal to distal):
- Prostatic urethra:
- Begins as a continuation of the bladder neck and passes through the prostate gland.
- Receives the ejaculatory ducts (containing spermatozoa from the testes and seminal fluid from the seminal vesicle glands) and the prostatic ducts (containing alkaline fluid).
- It is the widest and most dilatable portion of the urethra.
- Membranous urethra:
- Passes through the pelvic floor and the deep perineal pouch.
- Surrounded by the external urethral sphincter – which provides voluntary control of micturition.
- It is the narrowest and least dilatable portion of the urethra.
- Penile (bulbous) urethra:
- Passes through the bulb and corpus spongiosum of the penis, ending at the external urethral orifice (the meatus).
- Receives the bulbourethral glands proximally.
- In the glans (head) of the penis, the urethra dilates to form the navicular fossa.
Note: The part of the urethra that passes through the bladder neck is considered by some authors as a fourth anatomic part of the urethra.
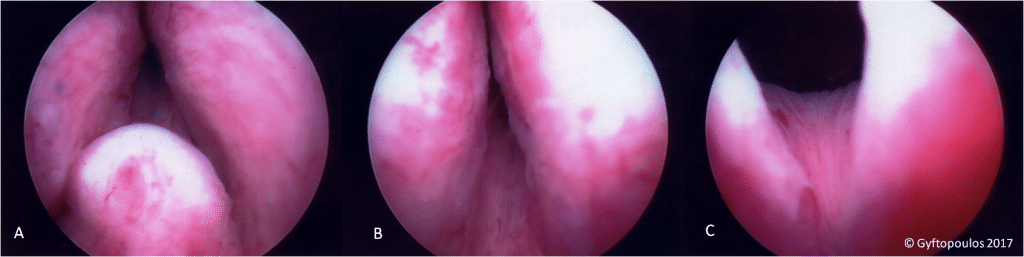
Fig 2 – Endoscopic view of the prostatic urethra from the entrance of the ejaculatory ducts (A) towards the bladder neck (C).
Neurovascular Supply
The arterial supply to the male urethra is via several arteries:
- Prostatic urethra – supplied by the inferior vesical artery (branch of the internal iliac artery which also supplies the lower part of the bladder).
- Membranous urethra – supplied by the bulbourethral artery (branch of the internal pudendal artery)
- Penile urethra – supplied directly by branches of the internal pudendal artery.
The nerve supply to the male urethra is derived from the prostatic plexus, which contains a mixture of sympathetic, parasympathetic and visceral afferent fibres.
Lymphatic Drainage
Lymphatic drainage also varies according to the region of the urethra. The prostatic and membranous portions drain to the obturator and internal iliac nodes, while the penile urethra drains to the deep and superficial inguinal nodes.
Clinical Relevance: Male Catheterisation
Urinary catheterisation is the process of inserting a tube through the urethra and into the bladder. This is typically performed in situations where urine output needs to be monitored (such as sepsis), or when the patient is unable to pass urine (urinary retention).
Catheterisation is more complex in males, as there are two angles to consider – the infrapubic and prepubic angles. The prepubic angle can be diminished by holding the penis upwards during urinary catheterisation.
It is also important to note the three constrictions in the male urethra – the internal urethral sphincter, external urethral sphincter, and external urethral orifice.
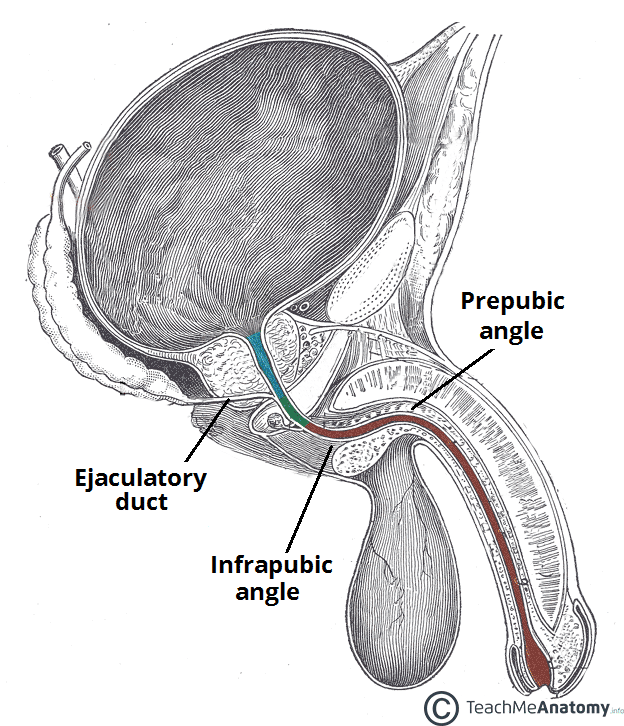
Fig 3 – The infrapubic and prepubic angles of the male urethra. The prepubic angle can be reduced by raising the penis during catheterisation.
Female Urethra
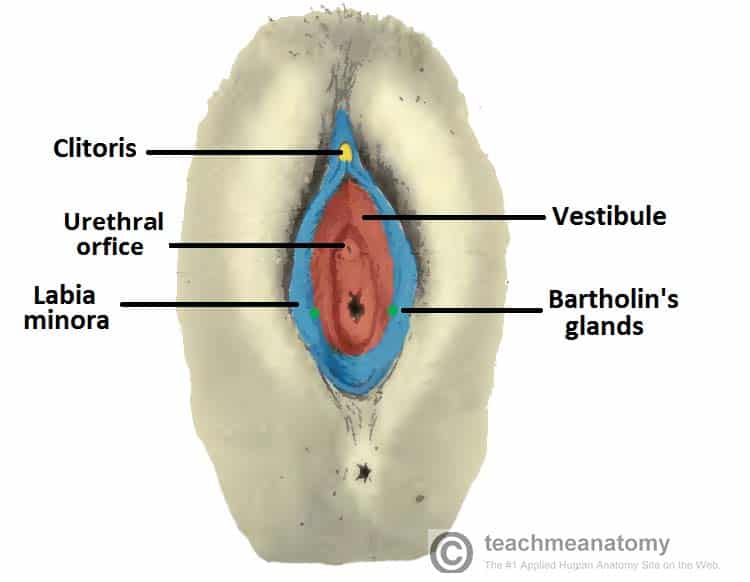
In females, the urethra is relatively short (approximately 4cm). It begins at the neck of the bladder, and passes inferiorly through the perineal membrane and muscular pelvic floor. The urethra opens directly onto the perineum, in an area between the labia minora, known as the vestibule.
Within the vestibule, the urethral orifice is located anteriorly to the vaginal opening, and 2-3cm posteriorly to the clitoris. The distal end of the urethra is marked by the presence of two mucous glands that lie either side of the urethra – Skene’s glands. They are homologous to the male prostate.
Neurovascular Supply
The arterial supply to the female urethra is via the internal pudendal arteries, vaginal arteries and inferior vesical branches of the vaginal arteries. Venous drainage is given by veins of the same names.
The nerve supply to the female urethra arises from the vesical plexus and the pudendal nerve. Visceral afferents from the urethra run in the pelvic splanchnic nerves.
Lymphatic Drainage
Lymphatic drainage of the proximal female urethra is to the internal iliac nodes, while the distal urethra drains to the superficial inguinal lymph nodes.
Clinical Relevance: Urinary Tract Infections
Due to the short length of the urethra, women are more susceptible to infections of the urinary tract. This usually manifests as cystitis, an infection of the bladder.
Common symptoms of cystitis are dysuria (pain upon urination), frequency, urgency, and haematuria (blood in the urine). A mid-stream urine sample can be tested for the presence of nitrites and leukocytes (both of which indicate infection).
Simple urinary tract infections are typically treated with a three-day course of antibiotics.