The spermatic cord refers to a collection of vessels, nerves and ducts that run to and from the testes. They are surrounded by fascia, forming a cord-like structure.
This article will look at the anatomy of the spermatic cord – its anatomical course, contents, and clinical correlations.
Anatomical Course
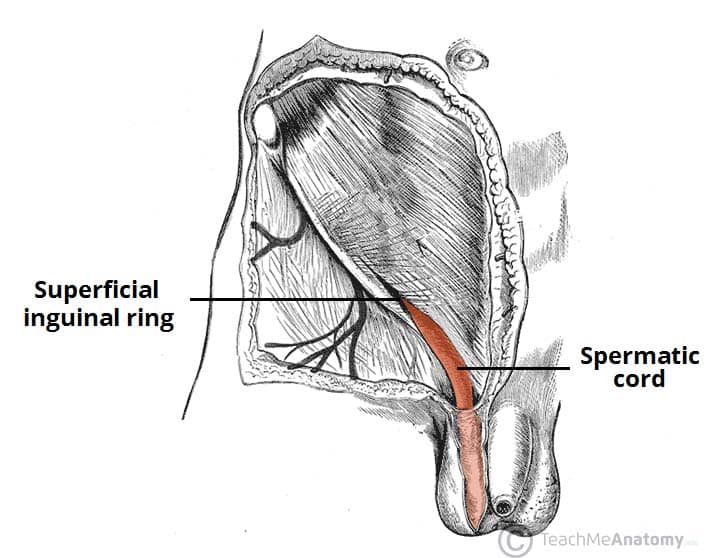
The anatomical course of the spermatic cord is relatively short, beginning in the inferior abdomen and ending in the scrotum.
The spermatic cord is formed at the opening of the inguinal canal, known as the deep inguinal ring. This opening is located laterally to the inferior epigastric vessels.
The cord passes through the inguinal canal, entering the scrotum via the superficial inguinal ring. It continues into the scrotum, ending at the posterior border of the testes. Here, its contents disperse to supply the various structures of the testes and scrotum.
Fascial Coverings
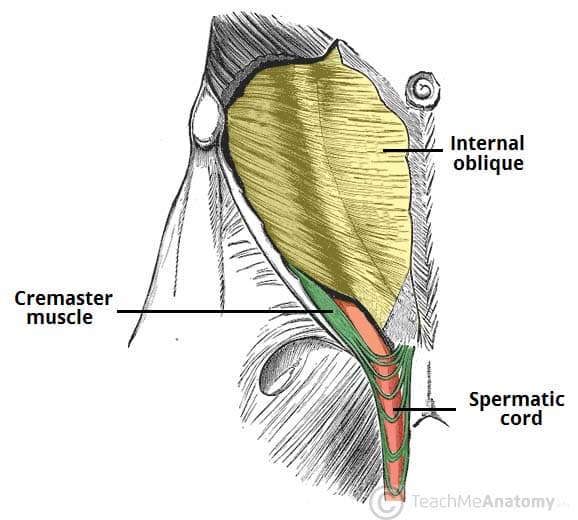
The contents of the spermatic cord are mainly bound together by three fascial layers. They are all derived from anterior abdominal wall:
- External spermatic fascia – derived from the aponeurosis of the external oblique muscle.
- Cremaster muscle and fascia – derived from the internal oblique muscle.
- Internal spermatic fascia – derived from the transversalis fascia.
The three fascial layers themselves are covered by a layer of superficial fascia, which lies directly below the scrotal skin.
The cremaster muscle forms the middle layer of the spermatic cord fascia. It is a discontinuous layer of striated muscle that is orientated longitudinally.
Clinical Relevance: Cremasteric Reflex
The cremasteric reflex can be stimulated by stroking the superior and medial part of the thigh. This produces an immediate contraction of the cremaster muscle, elevating the testis on the side that has been stimulated.
This spinal reflex consists of two parts:
- Afferent (sensory) limb – ilioinguinal nerve (innervates the skin of the superomedial thigh). Fibres from this nerve enter the spinal cord at L1.
- Efferent (motor) limb – genital branch of the genitofemoral nerve (innervates the cremaster muscle).
Contents
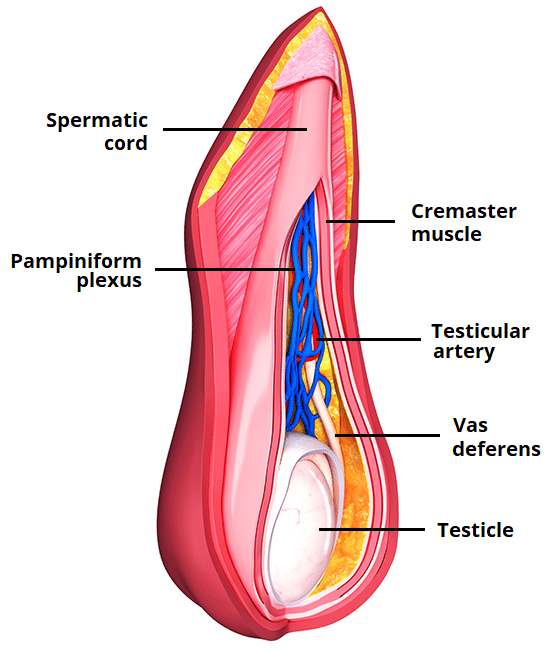
The spermatic cord conveys several important structures that run to and from the testis.
- Blood vessels:
- Testicular artery – branch of the aorta that arises just inferiorly to the renal arteries.
- Cremasteric artery and vein – supplies the cremasteric fascia and muscle.
- Artery to the vas deferens – branch of the inferior vesicle artery, which arises from the internal iliac.
- Pampiniform plexus of testicular veins – drains venous blood from the testes into the testicular vein.
- Nerves:
- Genital branch of the genitofemoral nerve – supplies the cremaster muscle.
- Autonomic nerves
- Other structures:
- Vas deferens – the duct that transports sperm from the epididymis to the ampulla (a dilated terminal part of the duct), ready for ejaculation.
- Processus vaginalis – projection of peritoneum that forms the pathway of descent for the testes during embryonic development. In the adult, it is fused shut.
- Lymph vessels – these drain into the para-aortic nodes, located in the lumbar region.
Pampiniform Plexus
The pampiniform plexus is a network of veins, responsible for the venous drainage of the testes. It has a unique configuration, wrapping itself around the testicular artery
The testes function best at a temperature just below that of the body. The pampiniform plexus acts as a heat exchanger, cooling the arterial blood before it reaches the testes. As it travels through the inguinal canal, the pampiniform plexus condenses into a single testicular vein.
The right testicular vein drains into the inferior vena cava and the left testicular vein drains into the left renal vein. However, there are also some anastomotic branches that allow communication with other veins, such as the cremasteric, scrotal and internal pudendal veins.
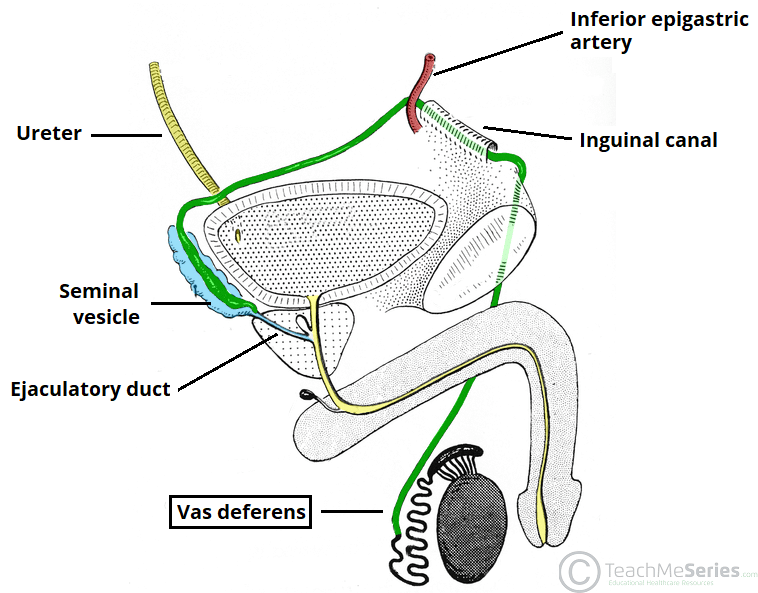
Vas Deferens
The vas deferens is a straight, thick muscular tube that conveys sperm from the epididymis to the ampulla and eventually, to the ejaculatory duct (formed by the convergence of the vas deferens and seminal vesicle duct). From the ejaculatory duct, sperm can pass through to the prostatic urethra.
The wall of the vas deferens consists largely of smooth muscle, arranged in three muscle layers:
| Inner Layer | Intermediate Layer |
Outer Layer |
|
|
|
There is a rich autonomic innervation of these muscle fibres, which permits fast movement of sperm towards the ejaculatory duct. This movement is also facilitated by the inner mucosal layer of the vas deferens – which is lined by cells that possess microvilli. Their seaweed-like movement helps advance spermatozoa through the spermatic tube.
The anatomical course of the vas deferens is as follows:
- It is continuous with the tail of the epididymis.
- Travels through the inguinal canal, as part of the spermatic cord.
- Moves down the lateral pelvic wall close to the ischial spine.
- Turns medially to pass between the bladder and the ureter and then travels downward on the posterior surface of the bladder.
- The inferior narrow part of the ampulla joins the duct from the seminal vesicle to form the ejaculatory duct.
Clinical Relevance: Testicular Torsion
Testicular torsion is a surgical emergency, where the spermatic cord twists upon itself. This can lead to strangulation of the testicular artery, resulting in necrosis of the testis.
A common cause of testicular torsion is spasm of the cremasteric muscle fibres which then force the testicle to spin around its own cord. Certain anatomic conditions (e.g. a loose testicle in a large peritoneal sac – tunica vaginalis) may facilitate this movement.
Diagnosis can be confirmed via ultrasound and colour doppler scanning. The main clinical feature of testicular torsion is severe, sudden pain in the affected testis which usually lies higher (due to the torsion of the cord) in the scrotum.
Testicular torsion is an absolute surgical emergency. A few hours delay can lead to testicular necrosis.