The seminal vesicles (also known as the vesicular or seminal glands) are a pair of glands found in the male pelvis, which function to produce many of the constituent ingredients of semen. They ultimately provide around 70% of the total volume of semen.
In this article we will consider the anatomical relations, functions, neurovascular relations and clinical significance of the seminal vesicles.
Anatomical Position and Structure
The seminal glands are a pair of 5cm long tubular glands. They are located between the bladder fundus and the rectum (separated from the latter by the rectovesicle pouch and the rectoprostatic fascia).
Their most important anatomical relation is with the vas deferens, which combine with the duct of the seminal vesicles to form the ejaculatory duct, which subsequently drains into the prostatic urethra.
Internally the gland has a honeycombed, lobulated structure with a mucosa lined by pseudostratified columnar epithelium. These columnar cells are highly influenced by testosterone, growing taller with higher levels, and are responsible for the production of seminal secretions.
Embryology
The Seminal glands, along with the Ejaculatory ducts, Epididymis and Ductus (vas) deferens, are derived from the mesonephric ducts, the precursor structure of male internal genitalia.
These structures can easily be remembered using the acronym SEED.

Fig 1.0 – Anatomical position of the seminal vesicles in relation to the vas deferens and prostate.
Function
The secretions of the seminal gland have a key role in the normal functioning of semen, making up 70% of its total volume.
It is notable however that the first fractions of expelled semen contain mainly spermatozoa and prostatic secretions; the fluids from the seminal vesicles are included in the late ejaculate fractions. These fluids contain:
- Alkaline fluid – neutralises the acidity of the male urethra and vagina in order to facilitate the survival of spermatozoa.
- Fructose – provides an energy source for spermatozoa.
- Prostaglandins – have a role in suppressing the female immune response to foreign semen.
- Clotting factors – designed to keep semen in the female reproductive tract post-ejaculation.
The remaining volume of semen is made up of testicular spermatozoa, prostatic secretions and mucus from the bulbourethral gland.
Vasculature
The arteries to the seminal gland are derived from the inferior vesicle, internal pudendal and middle rectal arteries, all of which stem from the internal iliac artery.
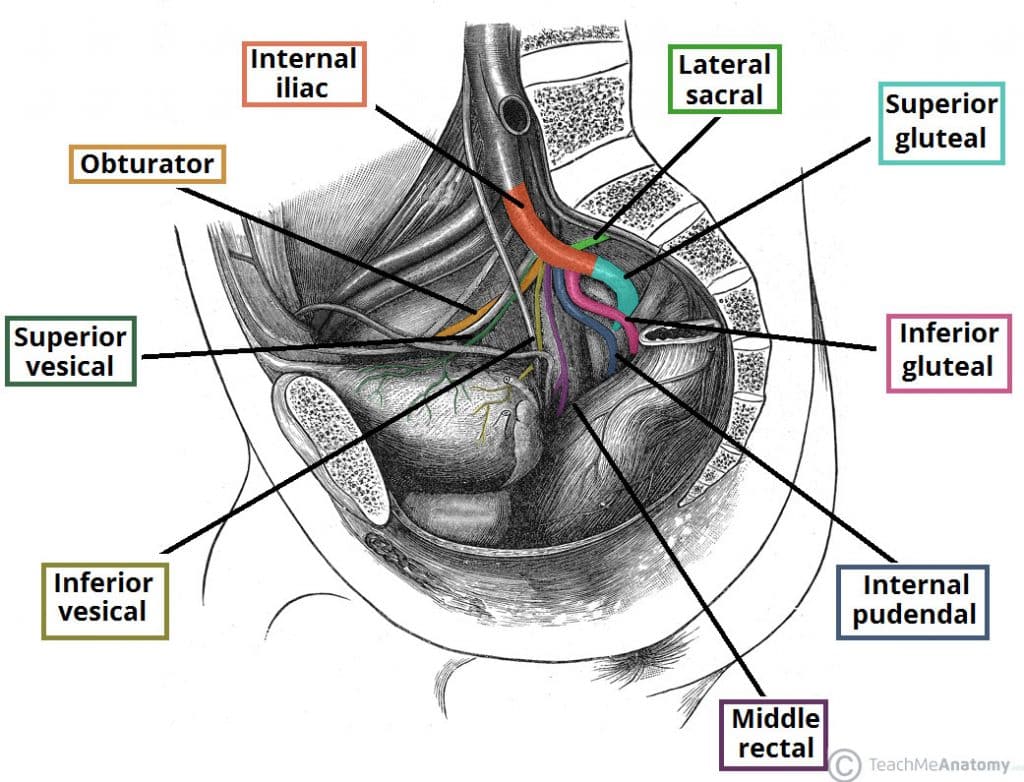
Fig 2 – The major branches of the internal iliac artery. Note that the anterior and posterior trunks are not visible in this illustration.
Innervation
The innervation of the gland, like much of the male internal genitalia, is mainly sympathetic in origin.
You can use the classic memory aid Point and Shoot to remember this. Erection, or pointing, receives parasympathetic innervation, while ejaculation (including contraction of the smooth muscle of the seminal vesicles) receives sympathetic innervation.
Lymphatic Drainage
The lymphatic drainage of the gland is the external and internal iliac lymph nodes.
Clinical Relevance – Seminal Gland Abscess
Inflammation of the seminal vesicles (also known as vesiculitis or spermatocystitis) may result after microbial infection of the urethra and prostate gland. Symptoms such as vague perineal or penile pain, discomfort during ejaculation and haemospermia (blood in the ejaculate) are suggestive of such infection.
Treatment consists of proper antibiotic regimens. In rare cases, obstruction of the seminal vesicle duct may lead to abscess formation. In such cases paracentesis is the mainstay of treatment. Drainage of these abscesses may be facilitated by transrectal ultrasound (TRUS) guided aspiration.
Clinical Relevance – Examination and Investigation
Physical examination of the seminal glands through digital rectal examination (DRE) is difficult.
A laboratory investigation of fructose levels in a sperm specimen may provide indirect evidence of seminal vesicle dysfunction, obstruction or congenital absence.