The pelvic viscera (bladder, rectum, pelvic genital organs and terminal part of the urethra) reside within the pelvic cavity (or the true pelvis). This cavity is located within the lesser part of the pelvis, beneath the pelvic brim.
A number of muscles help make up the walls of the cavity – the lateral walls include the obturator internus and the piriformis muscle, with the latter also forming the posterior wall
In this article, we shall look at the anatomy of the muscles that make up the inferior lining of the cavity – the pelvic floor muscles. The pelvic floor is also known as the pelvic diaphragm.
We shall look at the individual roles of these muscles, their innervation and blood supply, and any clinical correlations.
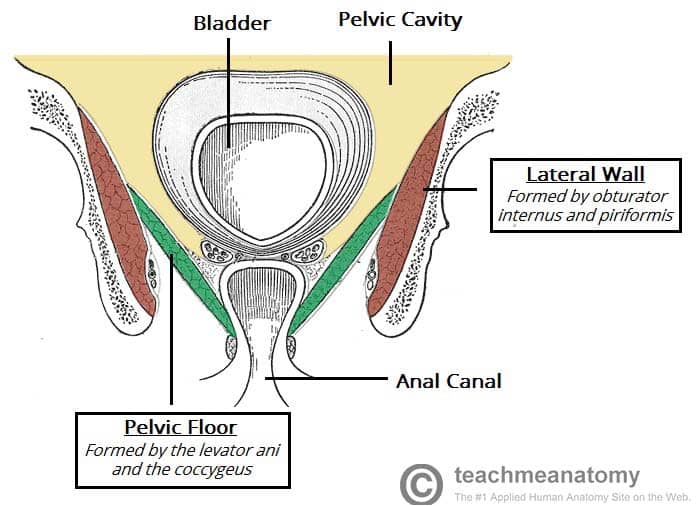
Fig 1 – An overview of the pelvic cavity and its walls. Note the funnel shape of the pelvic floor.
Note – some texts consider the pelvic floor to include the perineal membrane and deep perineal pouch. We have considered these as a distinct and separate structures.
Pelvic Floor Structure
The pelvic floor is a funnel-shaped structure. It attaches to the walls of the lesser pelvis, separating the pelvic cavity from the perineum inferiorly (region which includes the genitalia and anus).
In order to allow for urination and defecation, there are a few gaps in the pelvic floor. There are two ‘holes’ that have significance:
- Urogenital hiatus – an anteriorly situated gap, which allows passage of the urethra (and the vagina in females).
- Rectal hiatus – a centrally positioned gap, which allows passage of the anal canal.
Between the urogenital hiatus and the anal canal lies a fibrous node known as the perineal body, which joins the pelvic floor to the perineum (described further here).
Functions
As the floor of the pelvic cavity, these muscles have important roles to play in the correct functioning of the pelvic and abdominal viscera.
The roles of the pelvic floor muscles are:
- Support of abdominopelvic viscera – through their tonic contraction.
- Resistance to increases in intra-pelvic/abdominal pressure – during activities such as coughing or lifting heavy objects.
- Urinary and faecal continence – the muscle fibres have a sphincter action on the rectum and urethra. They relax to allow urination and defecation.
Muscles
When learning about the muscles of the pelvic floor, it is important to keep in mind its funnel-shaped structure. There are three main components of the pelvic floor:
- Levator ani muscles (largest component).
- Coccygeus muscle.
- Fascia coverings of the muscles.
We shall now consider each of these components in more detail.
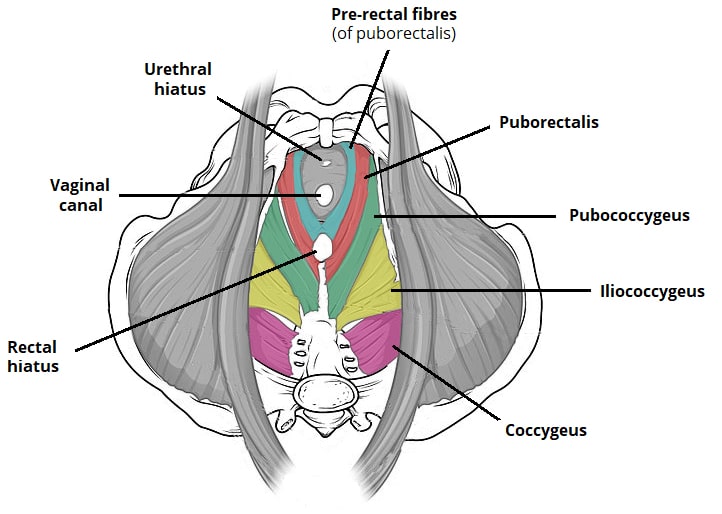
Fig 2 – Superior (bird’s eye) view of the pelvic floor. Note the pre-rectal fibres of the puborectalis.
Levator Ani Muscles
The levator ani is a broad sheet of muscle. It is composed of three separate paired muscles; pubococcygeus, puborectalis and iliococcygeus.
Puborectalis
The puborectalis is the most important of the levator ani group for maintaining faecal continence.
- Attachments: Originates from the posterior surface of the pubis. It forms a U-shaped sling around the anal canal, and attaches to the pubis on the contralateral side.
- Actions: Tonic contraction bends the anal canal anteriorly. This creates the anorectal angle which contributes to faecal continence. It is voluntarily inhibited during defecation.
- Innervation: Nerve to levator ani and pudendal nerve.
Some fibres of the puborectalis muscle (pre-rectal fibres) form another U-shaped sling that flank the urethra in the male and the urethra and vagina in the female (in some textbooks they appear as pubovaginalis or sphincter urethrae / vaginae). These fibres are very important in preserving urinary continence, especially during abrupt increase of the intra-abdominal pressure i.e. during sneezing.
Pubococcygeus
The pubococcygeus forms the bulk of the levator ani complex. It is located between the puborectalis and iliococcygeus within the pelvic floor.
- Attachments: Originates from the posterior surface of the pubis. It blends with the contralateral muscle in the midline of the pelvic floor.
- Actions: Stability and support of abdominal and pelvic organs.
- Innervation: Nerve to levator ani and branches of the pudendal nerve.
Iliococcygeus
The iliococcygeus is a thin muscle which forms the posterolateral part of the levator ani muscle group.
- Attachments: Originates from the ischial spines and the posterior tendinous arch of the internal obturator fascia. It inserts onto the coccyx, perineal body and anococcygeal ligament. It also blends with the fibres of the contralateral muscle in the midline of the pelvic floor.
- Actions: Elevates the pelvic floor and anorectal canal.
- Innervation: Nerve to levator ani and branches of the pudendal nerve.
Coccygeus
The coccygeus is a small triangular muscle located posterior to the levator ani muscle group.
- Attachments: Originates from the ischial spines and inserts onto the inferior end of the sacrum and coccyx.
- Actions: Supports the pelvic viscera and flexes the coccyx.
- Innervation: Anterior rami of S4 and S5.
- Blood supply: Inferior vesical, inferior gluteal and pudendal arteries.
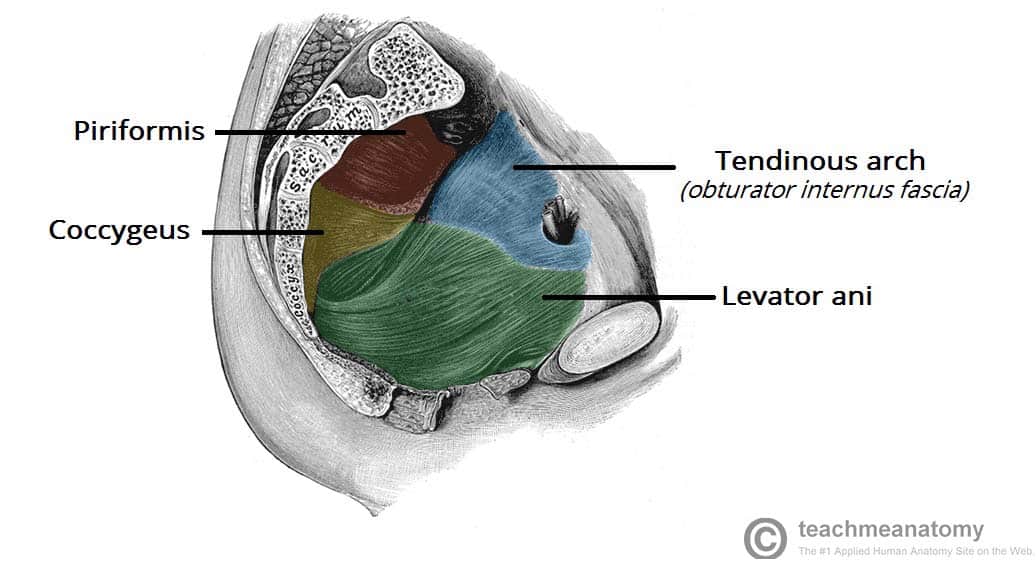
Fig 3 – Sagittal cut through the pelvis, showing a lateral view of the pelvic floor and walls.
Clinical Relevance: Pelvic Floor Dysfunction
Pelvic floor dysfunction refers to a range of signs and symptoms that related to abnormal functioning of the pelvic floor muscles.
In women, the pelvic floor muscles support the urethra, vagina, and anal canal. The weakening of these muscles can result in a loss of structural support to these organs – presenting as:
- Urinary incontinence
- Faecal incontinence
- Genitourinary prolapse
- Pelvic pain
- Sexual dysfunction
The causes of pelvic floor dysfunction are understood to be multifactorial and include obstetric trauma, increasing age, obesity, and chronic straining.