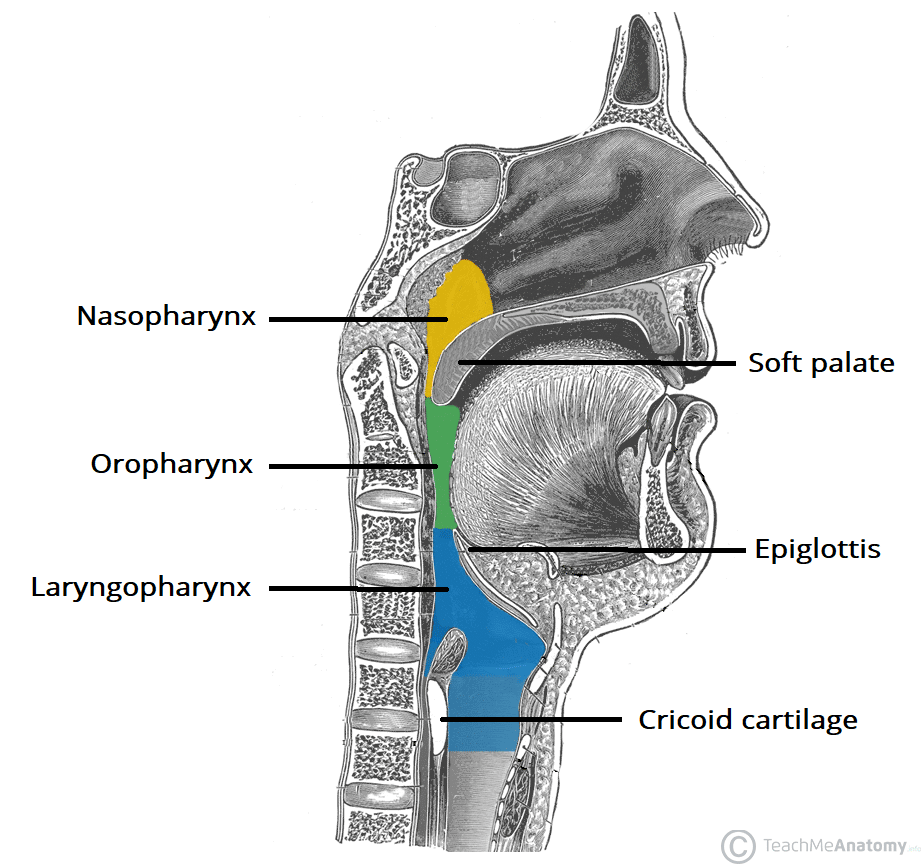
The pharynx is a muscular tube that connects the oral and nasal cavity to the larynx and oesophagus.
It begins at the base of the skull and ends at the inferior border of the cricoid cartilage (C6). The pharynx is comprised of three parts (superior to inferior):
- Nasopharynx
- Oropharynx
- Laryngopharynx.
In this article, we shall look at the anatomy of the pharynx – its structure, neurovascular supply, and any clinical correlations.
Nasopharynx
The nasopharynx is found between the base of the skull and the soft palate. It is continuous with the nasal cavity and performs a respiratory function by conditioning inspired air and propagating it into the larynx.
This part of the pharynx is lined with respiratory epithelium; ciliated pseudostratified columnar epithelium with goblet cells.
The posterosuperior nasopharynx contains the adenoid tonsils, which enlarge between 3-8 years of age and then regress.
Clinical Relevance: Enlarged Adenoid Tonsils
The adenoid tonsils can become pathologically enlarged due to viral infections of the upper respiratory tract. In the case of recurrent infections, they can become chronically enlarged. When enlarged, the adenoids can obstruct the opening of the Eustachian tube – which is located close to the adenoid tonsils in the nasopharynx.
Chronic obstruction of the Eustachian tube prevents the equalising of pressure in the middle ear with the atmosphere and normal drainage of fluid. This can lead to chronic otitis media with effusion, colloquially known as glue ear. In this condition, the static fluid and negative pressure in the middle ear provide the ideal environment for infection.
Oropharynx
The oropharynx is the middle part of the pharynx, located between the soft palate and the superior border of the epiglottis.
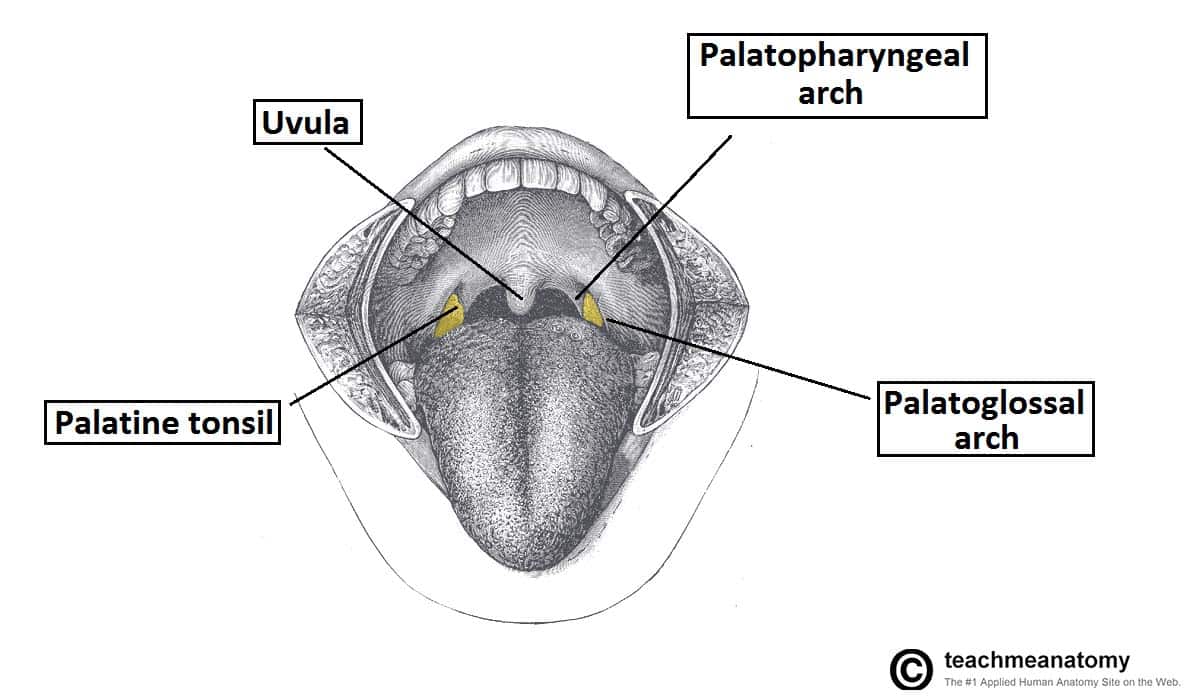
It contains the following structures:
- Posterior one-third of the tongue.
- Lingual tonsils – lymphoid tissue at the base of the tongue.
- Palatine tonsils – lymphoid tissue located in the tonsillar fossa (between the palatoglossal and palatopharyngeal arches of the oral cavity).
- Superior constrictor muscle
Waldeyer’s ring is the ring of lymphoid tissue in the naso- and oropharynx formed by the paired palatine tonsils, the adenoid tonsils and lingual tonsil.
The oropharynx is involved in the voluntary and involuntary phases of swallowing.
Laryngopharynx
The most distal part of the pharynx, the laryngopharynx is located between the superior border of the epiglottis and inferior border of the cricoid cartilage (C6). It is continuous inferiorly with the oesophagus.
It is found posterior to the larynx and communicates with it via the laryngeal inlet, lateral to which one can find the piriform fossae.
The laryngopharynx contains the middle and inferior pharyngeal constrictors.
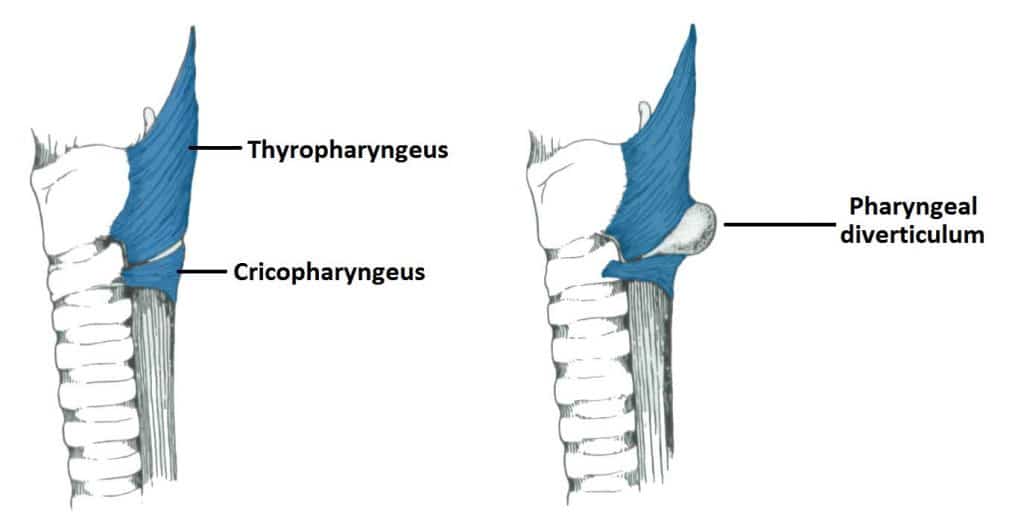
Clinical Relevance: Pharyngeal Diverticulum (Pouch)
The inferior pharyngeal constrictor is split into two parts; the thyropharyngeus and the cricopharyngeus. This area between the two is a weak area in the mucosa.
Normally during swallowing, the thyropharyngeus contracts as the cricopharyngeus relaxes, allowing the bolus of food to be propelled into the oesophagus and preventing the intrapharyngeal pressure from rising.
If this coordinated relaxation of the cricopharyngeus does not occur, the intrapharyngeal pressure tends to rise and pharyngeal mucosa forms a midline diverticulum in the area between the thyropharyngeus and cricopharyngeus. It is possible for food to accumulate here, leading to dysphagia.
Muscles
There are two main groups of pharyngeal muscles; longitudinal and circular.
The muscles of the pharynx are mostly innervated by the vagus nerve – the only exception being the stylopharyngeus (glossopharyngeal nerve).
Circular
There are three circular pharyngeal constrictor muscles – superior, middle, and inferior. They are arranged like stacked glasses, which form an incomplete muscular circle around the pharynx.
The circular muscles contract sequentially from superior to inferior to constrict the pharyngeal lumen. and thus propel the bolus of food inferiorly into the oesophagus.
- Superior pharyngeal constrictor – the uppermost pharyngeal constrictor. It is located in the oropharynx.
- Originates from the pterygomandibular ligament, alveolar process of mandible, medial pterygoid plate and pterygoid hamulus of the sphenoid bone.
- Inserts posteriorly onto the pharyngeal tubercle of the occiput and the pharyngeal raphe.
- Middle pharyngeal constrictor – located in the laryngopharynx.
- Originates from the stylohyoid ligament and the horns of the hyoid bone.
- Inserts posteriorly into the pharyngeal raphe.
- Inferior pharyngeal constrictor – located in the laryngopharynx. It has two components:
- Thyropharyngeal fibres originate from the thyroid cartilage
- Cricopharyngeal fibres originate from the cricoid cartilage
- All fibres insert posteriorly onto the pharyngeal raphe.
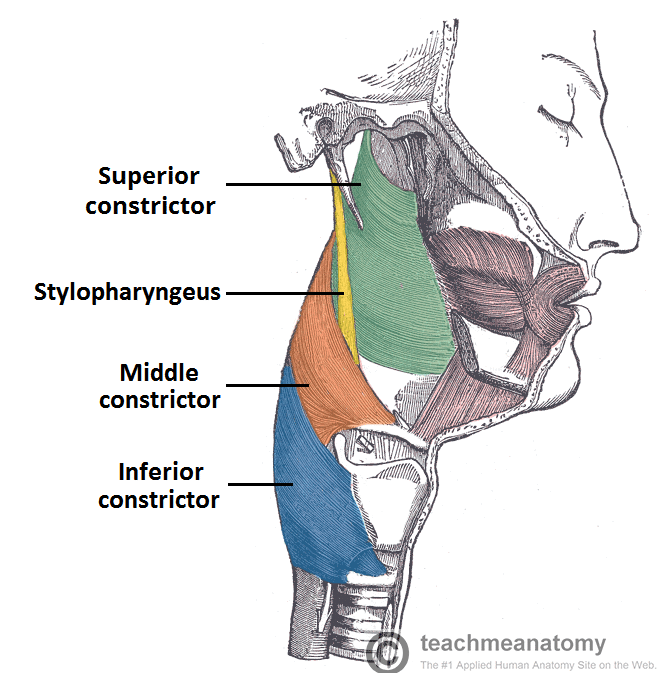
Fig 4 – Lateral view of the deep structures of the pharynx. Visible are the circular muscles of the pharynx, and the stylopharyngeus.
Longitudinal
The longitudinal muscles are the stylopharyngeus, palatopharyngeus and salpingopharyngeus. They act to shorten and widen the pharynx, and elevate the larynx during swallowing.
- Stylopharyngeus – originates from the styloid process of the temporal bone and inserts onto the pharyngeal wall.
- Unlike the other pharyngeal muscles, it is innervated by the glossopharyngeal nerve (CN IX).
- Palatopharyngeus – originates from the hard palate of the oral cavity and inserts onto the pharyngeal wall.
- Innervated by the vagus nerve (CN X).
- Salpingopharyngeus – originates from the Eustachian tube and inserts onto the pharyngeal wall.
- Innervated by the vagus nerve (CN X).
- In addition to contributing to swallowing, it also opens the Eustachian tube to equalise the pressure in the middle ear.
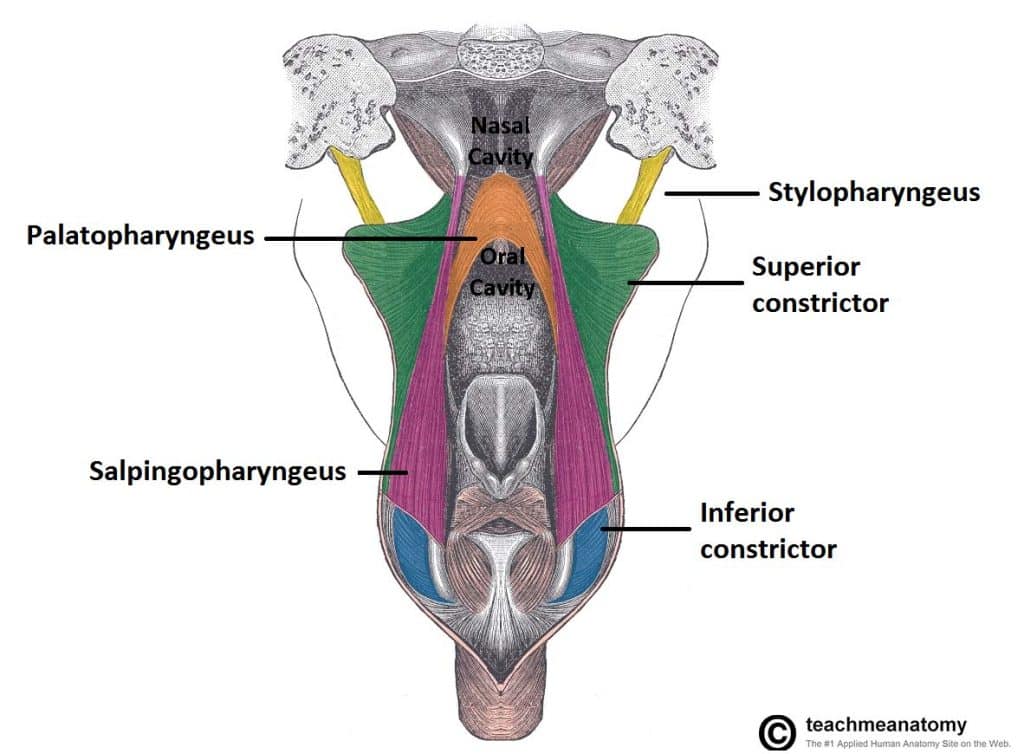
Fig 5 – Posterior view of the pharynx. The pharynx has been split down the midline and opened, to show the longitudinal muscles.
Innervation
Motor and sensory innervation of the majority of the pharynx (except nasopharynx) is achieved by the pharyngeal plexus.
The pharyngeal plexus, which overlies the middle pharyngeal constrictor, is formed by:
- Pharyngeal branches from the glossopharyngeal nerve (CN IX).
- Pharyngeal branch of the vagus nerve (CN X).
- Branches from the external laryngeal nerve.
- Sympathetic fibres from the superior cervical ganglion.
Sensory
The pharynx receives sensory innervation from the glossopharyngeal nerve.
In addition:
- The anterior and superior aspect of the nasopharynx is innervated by the maxillary nerve (CN V2)
- The inferior aspect of the laryngopharynx (surrounding the beginning of the larynx) is innervated by the internal branch of the vagus nerve.
Motor
All the muscles of the pharynx are innervated by the vagus nerve (CN X), except for the stylopharyngeus, which is innervated by the glossopharyngeal nerve (CN IX).
Vasculature
Arterial supply to the pharynx is via branches of the external carotid artery:
- Ascending pharyngeal artery
- Branches of the facial artery
- Branches of the lingual and maxillary arteries.
Venous drainage is achieved by the pharyngeal venous plexus, which drains into the internal jugular vein.
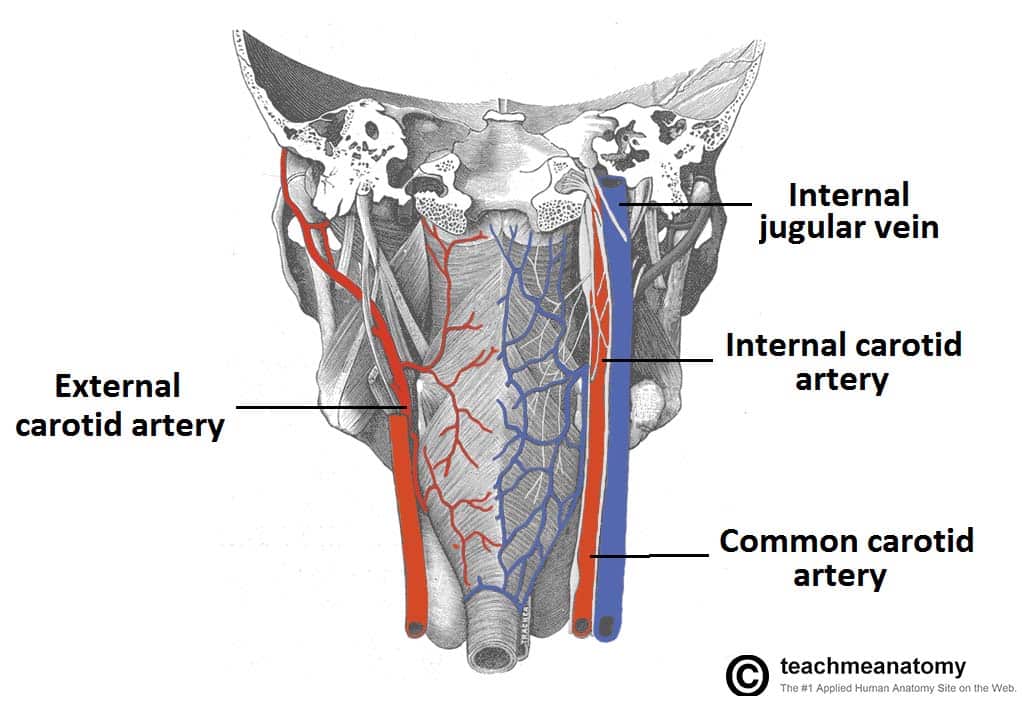
Fig 6 – Vasculature of the pharynx. Right arterial supply via the ECA and left venous plexus shown.