The head and neck receives the majority of its blood supply through the carotid and vertebral arteries.
In this article, we shall look at the anatomy of the arterial supply to the head and neck – its anatomical course, branches, and clinical correlations.
Carotid Arteries
We shall start at the origin of the carotid arteries. The right common carotid artery arises from a bifurcation of the brachiocephalic trunk (the right subclavian artery is the other branch). This bifurcation occurs roughly at the level of the right sternoclavicular joint.
The left common carotid artery branches directly from the arch of aorta. The left and right common carotid arteries ascend up the neck, lateral to the trachea and the oesophagus. They do not give off any branches in the neck.
At the level of the superior margin of the thyroid cartilage (C4), the carotid arteries split into the external and internal carotid arteries. This bifurcation occurs in an anatomical area known as the carotid triangle.
The common carotid and internal carotid are slightly dilated here, this area is known as the carotid sinus, and is important in detecting and regulating blood pressure.
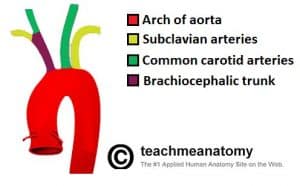
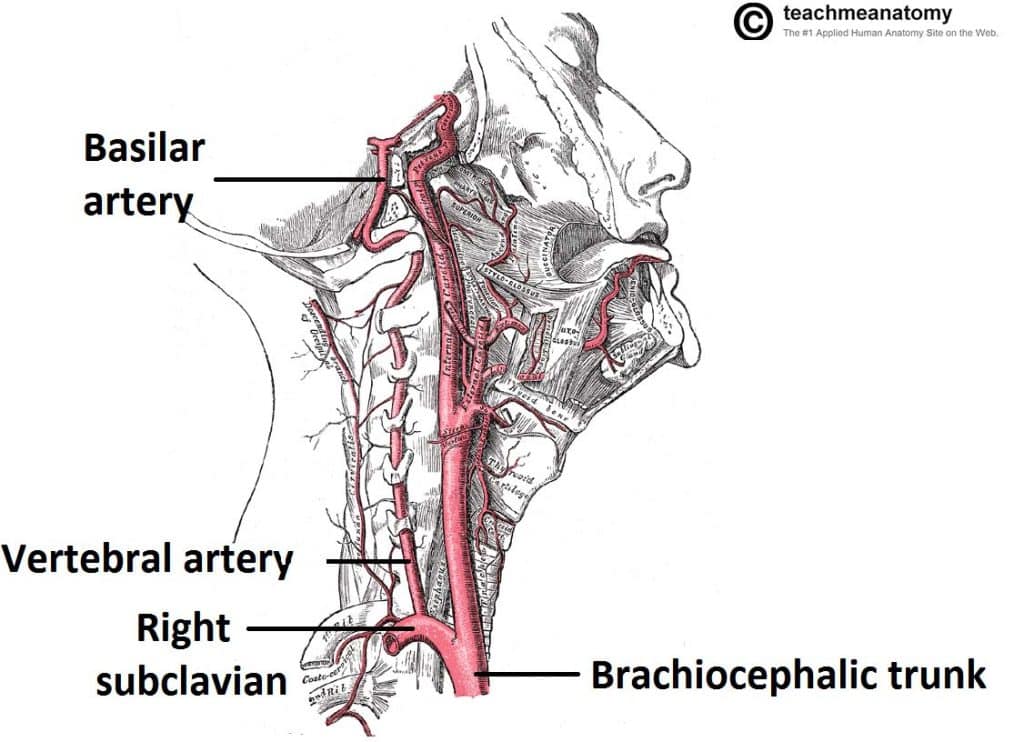
Fig 1.0 – Origin of the blood vessels of the upper limb. Note how the left common carotid and subclavian arteries arise directly from the arch of aorta.
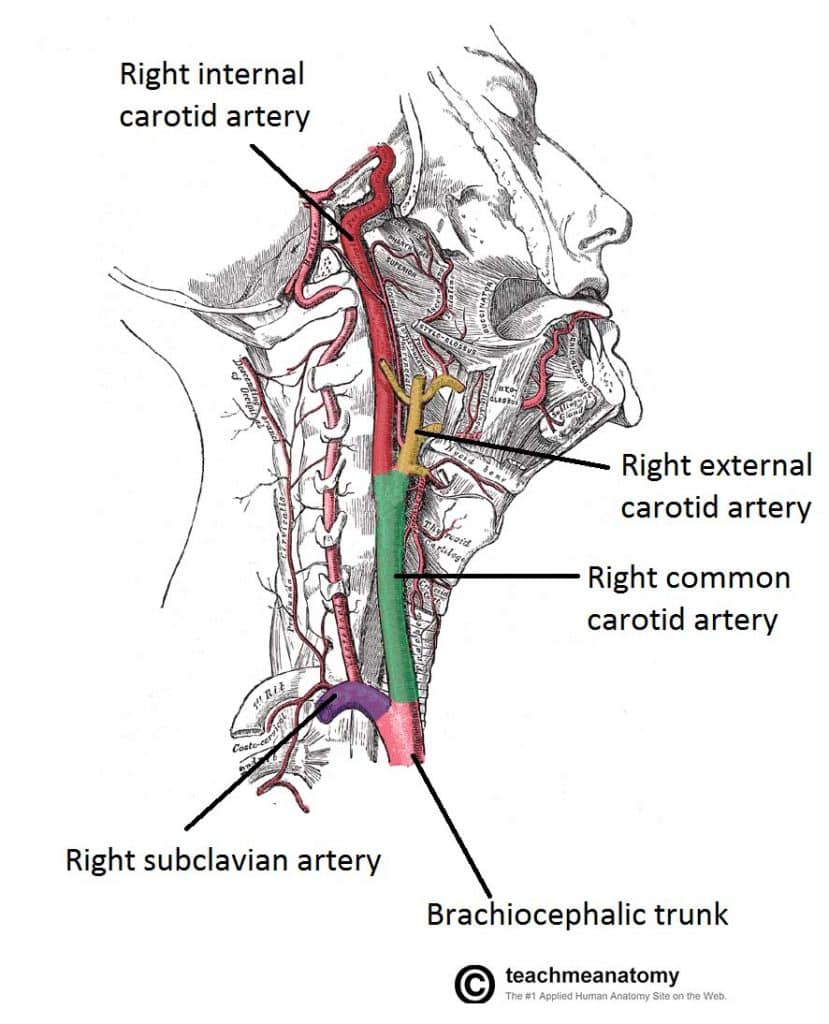
Fig 1.1 – Lateral vein of the neck, showing the origin and bifurcation of the common carotid artery.
Clinical Relevance: Carotid Sinus Hypersensitivity
The carotid sinus is a dilated portion of the common carotid artery and proximal internal carotid artery. It contains specialised sensory cells known as baroreceptors. These cells detect stretch as a measure of blood pressure. The glossopharyngeal nerve feeds this information to the brain, and this is used to regulate blood pressure.
In some individuals, the baroreceptors are hypersensitive to stretch. External pressure on the carotid sinus can cause slowing of the heart rate and a decrease in blood pressure. The brain becomes under-perfused and syncope results. In such patients, checking the pulse at the carotid triangle is not advised.
External to the carotid sinus, there is a cluster of nervous cells known as the carotid body. These cells act as peripheral chemoreceptors; detecting the O2 content of the blood and relaying this information to the brain to regulate breathing rate.
External Carotid Artery
The external carotid artery supplies the areas of the head and neck external to the cranium. After arising from the common carotid artery, it travels up the neck, passing posteriorly to the mandibular neck and anteriorly to the lobule of the ear.
The artery ends within the parotid gland by dividing into the superficial temporal artery and the maxillary artery. It gives rise to six branches in total:
- Superior thyroid artery
- Lingual artery
- Facial artery
- Ascending pharyngeal artery
- Occipital artery
- Posterior auricular artery
The facial, maxillary and superficial temporal arteries are the major branches of note. The maxillary artery supplies the deep structures of the face, while the facial and superficial temporal arteries generally supply superficial areas of the face.
Clinical Relevance: Blood Supply to the Scalp
The posterior auricular, occipital and superficial temporal arteries (along with two branches of the internal carotid artery; supra-orbital and supratrochlear) combine to provide a dense blood supply to the scalp. Injuries to the scalp can cause excessive bleeding for various reasons:
- The walls of the arteries are tightly and closely bound to the underlying connective tissue of the scalp. This prevents them from constricting to limit blood loss following injury or laceration.
- The numerous anastomoses formed by the arteries produce a very densely vascularised area.
- Deep lacerations can involve the epicranial aponeurosis, which is worsened by the opposing pulls of the occipital and frontalis muscles.
Despite the possible heavy bleeding, it is important to note that the bony skull gets its blood from an alternative source (middle meningeal artery), and so will not undergo avascular necrosis.
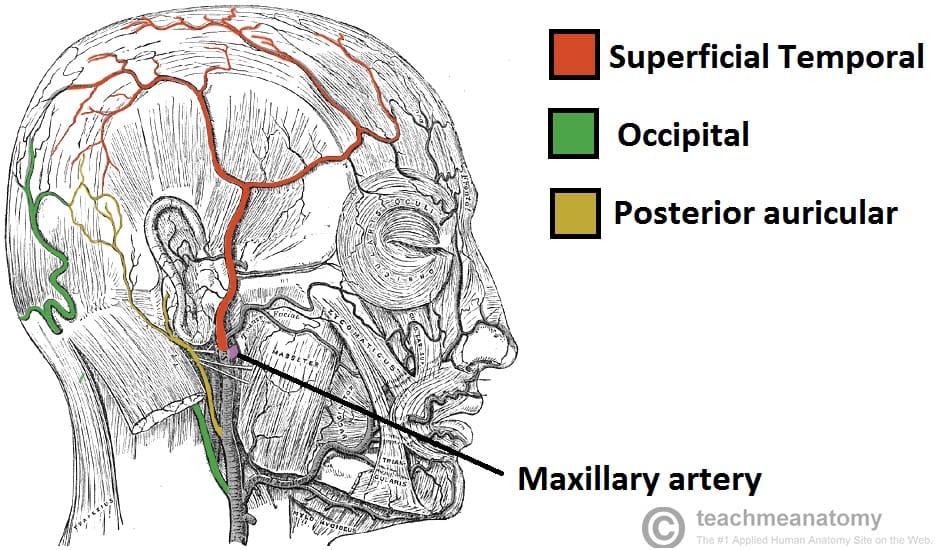
Fig 1.2 – Blood supply to the superficial structures of the face. Note the maxillary artery before it disappears into the pterygopalatine fossa, to supply the deep structures of the face.
Clinical Relevance: Extradural Haematoma
The middle meningeal artery is a branch of the maxillary artery. It is unique as it supplies some intracranial structures (remember, the external carotid artery and its branches usually supply extra-cranial structures).
The middle meningeal artery supplies the skull and the dura mater (the outer membranous layer covering the brain). A fracture of the skull at its weakest point, the pterion, can injure or completely lacerate the MMA. Blood will then collect in between the dura mater and the skull, causing a dangerous increase in intra-cranial pressure. This is known as an extradural haematoma.
The increase in intra-cranial pressure causes a variety of symptoms: nausea, vomiting, seizures, bradycardia and limb weakness. It is treated by diuretics in minor cases, and drilling burr holes into the skull the more extreme haemorrhages.
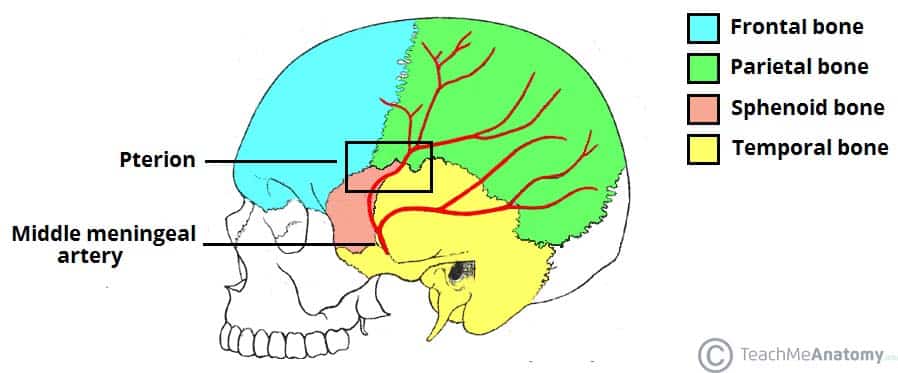
Fig 1.3 – Lateral view of the skull, showing the path of the meningeal arteries. Note the pterion, a weak point of the skull, where the anterior middle meningeal artery is at risk of damage.
Internal Carotid Artery
The internal carotid arteries do not supply any structures in the neck, entering the cranial cavity via the carotid canal in the petrous part of the temporal bone. Within the cranial cavity, the internal carotid artery supplies:
- The brain
- Eyes
- Forehead
Clinical Relevance: Atherosclerosis of the Carotid Arteries
The swelling at the bifurcation of the common carotid arteries, the carotid sinus, produces turbulent blood flow. This increases the risk of atheroma formation in this area, with the internal carotid most susceptible.
Atherosclerotic thickening of the tunica intima of these arteries will reduce blood flow to the brain, resulting in the variety of neurological symptoms; headache, dizziness, muscular weakness. If blood flow is completely occluded, a cerebral ischaemia (stroke) results.
If atherosclerosis of the carotid arteries is suspected, a Doppler study can be used to assess the severity of any thickening. In severe cases, the artery can be opened, and the atheromatous tunica intima removed. This procedure is called a carotid endarterectomy.
Vertebral Arteries
The vertebral arteries are paired vessels which arise from the subclavian arteries, just medial to the anterior scalenes. They ascend the posterior aspect of the neck, passing through holes in the transverse processes of the cervical vertebrae (known as foramen transversarium).
The vertebral arteries enter the cranium via the foramen magnum and converge to form the basilar artery – which continues to supply the brain. The vertebral arteries do not supply any branches to the neck or other extra-cranial structures.
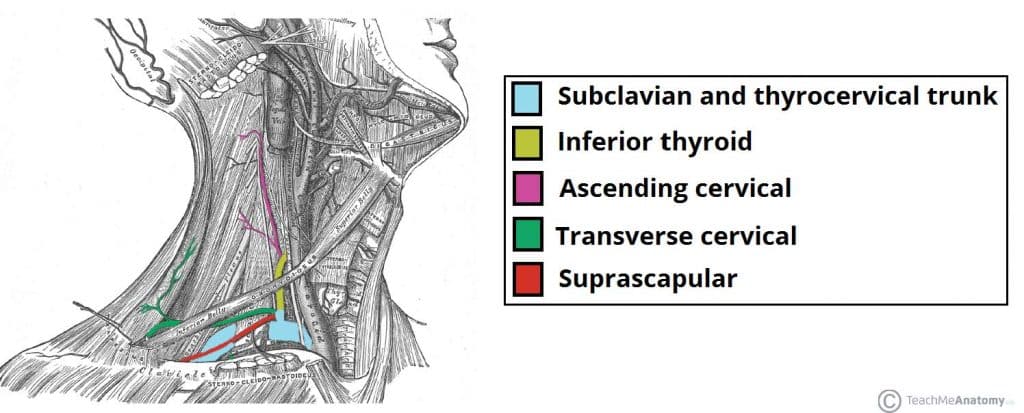
Other Arteries of the Neck
The neck is supplied by arteries other than the carotids. The right and left subclavian arteries give rise to the thyrocervical trunk. From this trunk, several vessels arise, which go on to supply the neck.
- The first branch of the thyrocervical trunk is the inferior thyroid artery. It supplies the thyroid gland
- The ascending cervical artery arises from the inferior thyroid artery, as it turns medially in the neck. This vessel supplies the posterior prevertebral muscles.
- The transverse cervical artery is the next branch off the thyrocervical trunk. It crosses the base of the carotid triangle and supplies the trapezius and rhomboid muscles.
- Lastly, the suprascapular artery arises. It supplies the posterior shoulder area.