The deep fibular nerve (deep peroneal nerve) is a nerve of the leg. It is one of the terminal branches of the common fibular nerve.
In this article, we shall look at the anatomy of the deep fibular nerve – its anatomical course, motor and sensory functions, and any clinical relevance.
Overview
- Nerve roots: L4-S2.
- Motor function: Innervates the muscles in the anterior compartment of the leg, as well as some of the intrinsic muscles of the foot.
- Sensory function: Supplies the triangular region of skin between the 1st and 2nd toes.
Anatomical Course
The deep fibular nerve is a terminal division of the common fibular nerve (itself a branch of the sciatic nerve). It arises within the lateral compartment of the leg, between the fibularis longus muscle and the neck of the fibula.
The nerve then travels medially, pierces the intermuscular septum, and enters the anterior compartment of the leg. Accompanied by the anterior tibial artery, it descends in a plane initially between the tibialis anterior and extensor digitorum longus, and then distally between the tibialis anterior and extensor hallucis longus. During its descent, the deep fibular nerve is initially lateral, then anterior and finally medial to the anterior tibial artery.
At the ankle, the deep fibular nerve travels underneath the extensor retinaculum. It then divides within the dorsum of the foot into two branches:
- Lateral branch – innervates two of the intrinsic muscles of the foot (extensor digitorum brevis and extensor hallucis brevis).
- Medial branch – innervates the skin of the webbed space between the 1st and 2nd toes.
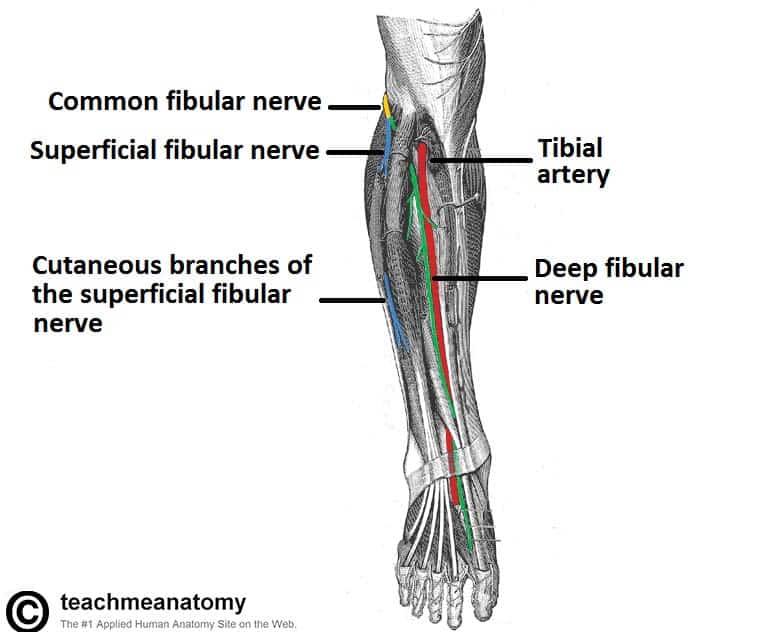
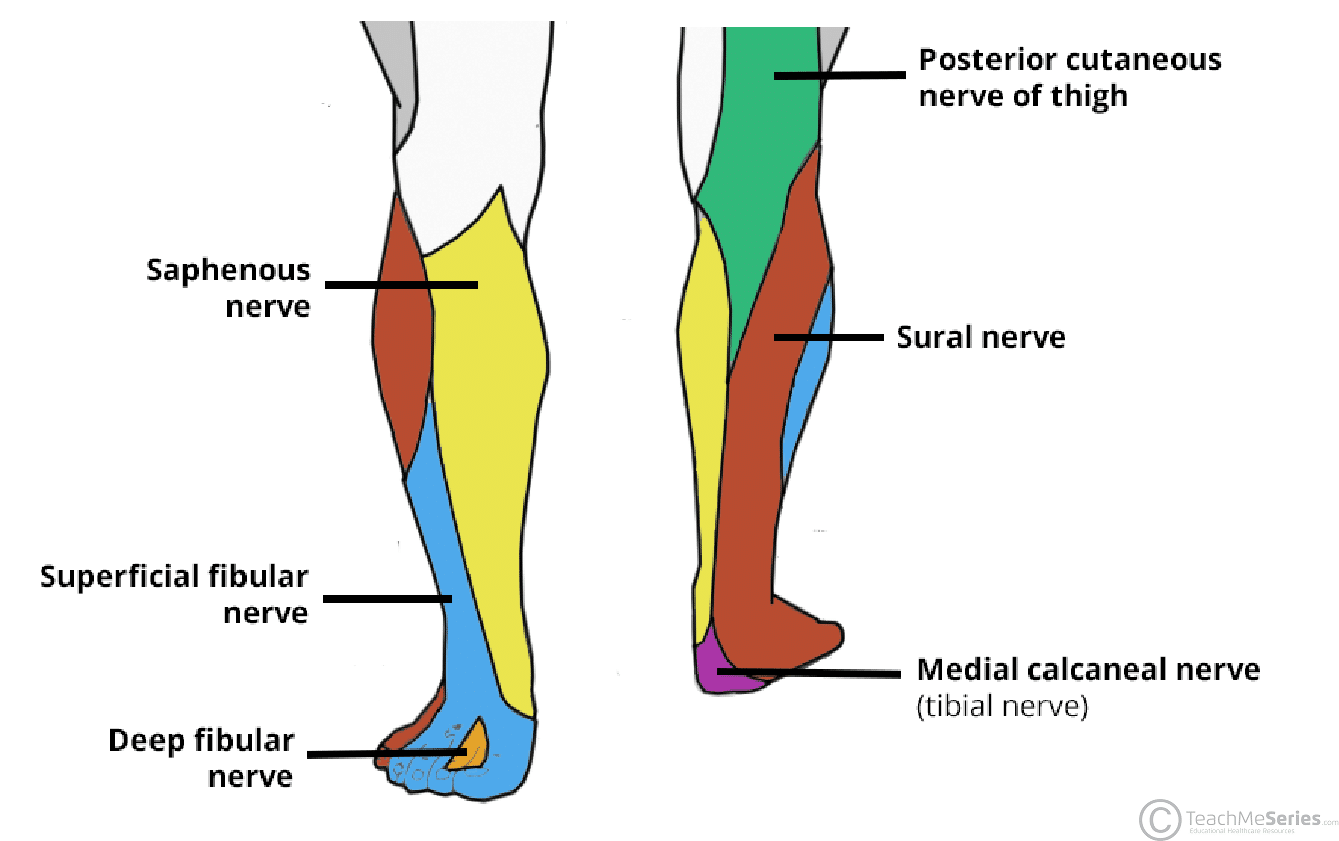
Fig 1 – Anterior view of the leg, showing the major nerves. The proximal portion of the fibularis longus has been removed to show the bifurcation of the common fibular nerve.
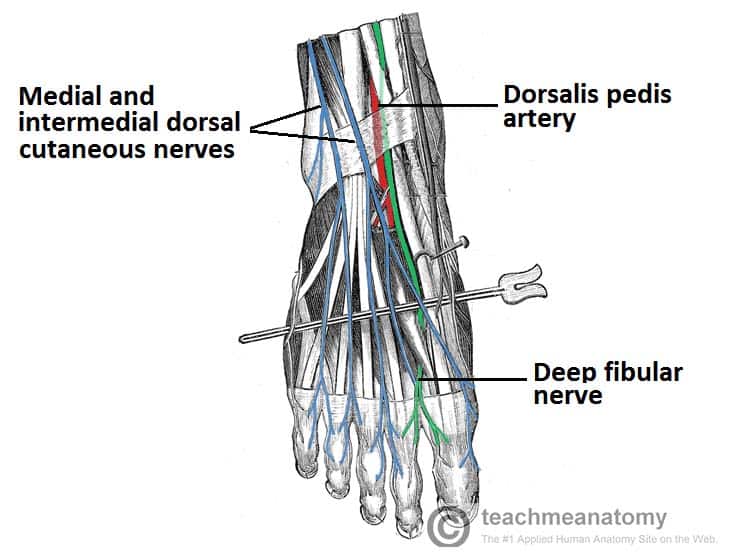
Fig 2 – The cutaneous nerves of the foot. Note the distribution of the dorsal cutaneous nerves
Motor Functions
The deep fibular nerve innervates the muscles in the anterior compartment of the leg, including:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- Fibularis tertius
These muscles are responsible for dorsiflexion of the foot at the ankle joint. During the gait cycle for walking, dorsiflexion is required:
- When a person strikes their heel on the floor in the stance phase.
- During the swing phase.
The deep fibular nerve also innervates the extensor digitorum brevis and extensor hallucis brevis, which are intrinsic muscles of the foot. These muscles are responsible for extending the toes at the metatarsophalangeal joints and interphalangeal joints.
Sensory Functions
The deep fibular nerve terminates in the dorsum of the foot as a cutaneous nerve.
It provides cutaneous innervation to the skin of the first webbed space on the dorsum of the foot.
Clinical Relevance – Footdrop
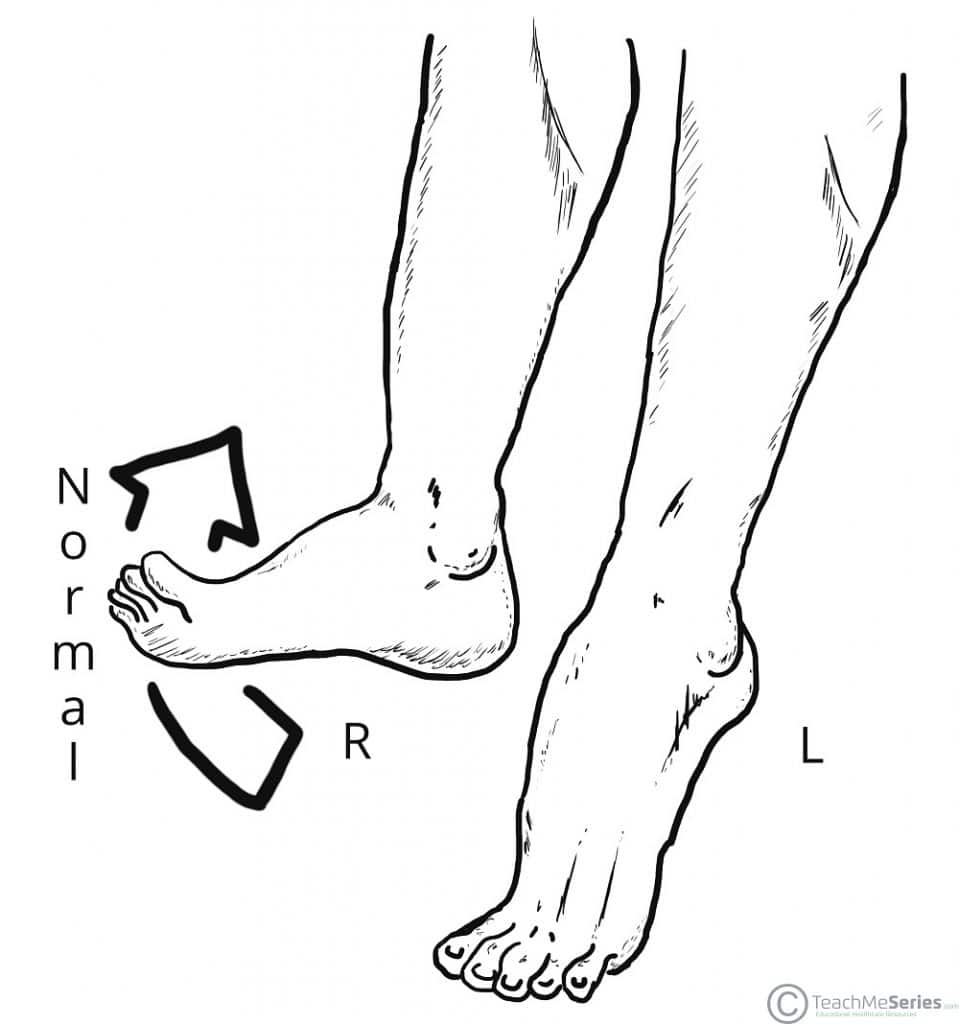
The deep fibular nerve can become entrapped or compressed during its course through the anterior compartment of the leg. This causes paralysis of the muscles in the anterior compartment of the leg, and so a patient loses the ability to dorsiflex the foot.
With unopposed plantarflexion, their foot drops. Footdrop gives the patient’s foot difficulty in clearing the ground during the swing phase of walking. In addition, the foot will slap down on the floor when the patient walks, because it can’t be lowered in a controlled manner.
There are two main reasons why the deep fibular nerve could be compressed.
- The first is that the anterior leg muscles have been excessively used and so are compressing the nerve within the anterior compartment. The patient will experience pain in the anterior leg.
- The other common cause is tight-fitting shoes, compressing the nerve beneath the extensor retinaculum. This commonly occurs with wearing tight ski boots (referred to as ski boot syndrome). The patient will also experience pain in the dorsum of the foot.