The parotid gland is a bilateral salivary gland located in the face.
It produces serous saliva – a watery solution rich in enzymes – which is then secreted into the oral cavity, where it lubricates and aids in the breakdown of food.
In this article, we shall look at the anatomy of the parotid gland – its location, neurovascular supply and any clinical correlations.
Anatomical Position
The parotid gland is a bilateral structure, which displays a lobular and irregular morphology. Anatomically, it can be divided into deep and superficial lobes, which are separated by the facial nerve.
It lies within a deep hollow, known as the parotid region. The parotid region is bounded as follows:
- Superiorly – Zygomatic arch.
- Inferiorly – Inferior border of the mandible.
- Anteriorly – Masseter muscle.
- Posteriorly – External ear and sternocleidomastoid.
The secretions of the parotid gland are transported to the oral cavity by the Stensen duct. It arises from the anterior surface of the gland, traversing the masseter muscle. The duct then pierces the buccinator, moving medially. It opens out into the oral cavity near the second upper molar.
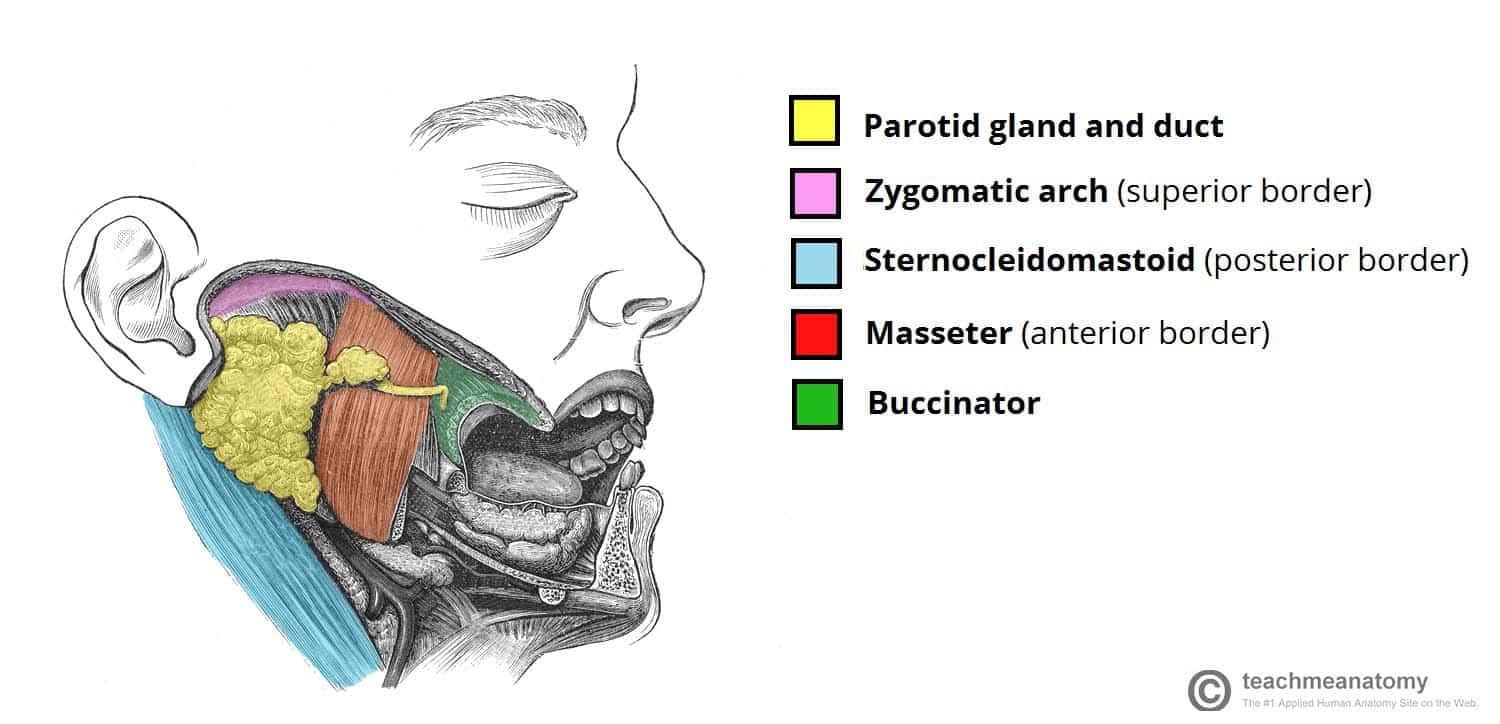
Fig 1 – Position of the parotid gland and borders of the parotid region.
Anatomical Relationships
The anatomical relationships of the parotid gland are of great clinical importance – particularly during parotid gland surgery.
Several important neurovascular structures pass through the gland:
- Facial nerve (CN VII) – gives rise to five terminal branches within the parotid gland. These branches innervate the muscles of facial expression.
- External carotid artery – gives rise to the posterior auricular artery within the parotid gland. It then divides into its two terminal branches – the maxillary artery and superficial temporal artery.
- Retromandibular vein – formed within the parotid gland by the convergence of the superficial temporal and maxillary veins. It is one of the major structures responsible for venous drainage of the face.
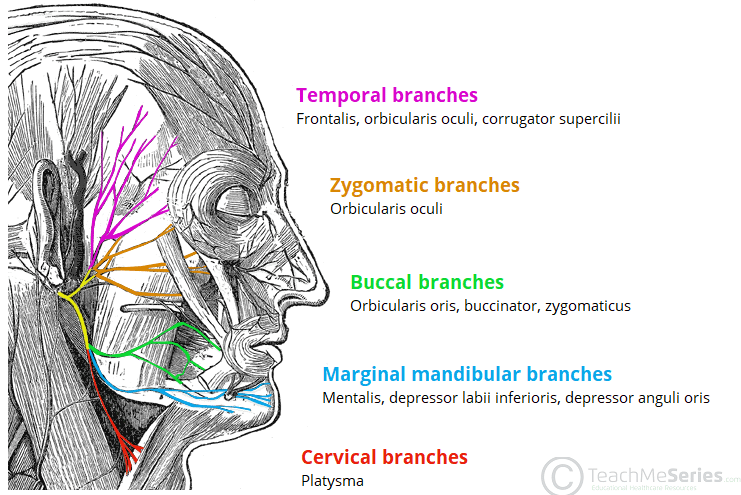
Fig 2 – Innervation to the muscles of facial expression via the facial nerve (CN VII)
Vasculature
Blood is supplied by the posterior auricular and superficial temporal arteries. They are both branches of the external carotid artery, which arise within the parotid gland itself.
Venous drainage is achieved via the retromandibular vein. It is formed by unification of the superficial temporal and maxillary veins.
Innervation
The parotid gland receives sensory and autonomic innervation. The autonomic innervation controls the rate of saliva production.
Sensory innervation is supplied by the auriculotemporal nerve (gland) and the great auricular nerve (fascia).
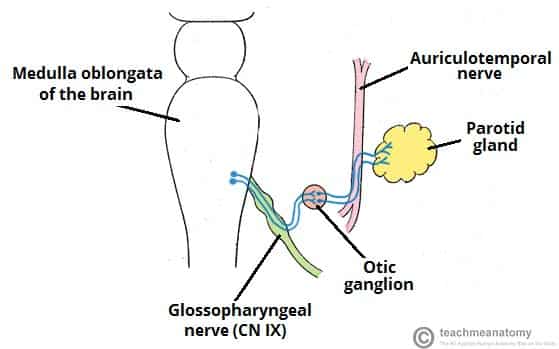
The parasympathetic innervation to the parotid gland has a complex path. It begins with the glossopharyngeal nerve (cranial nerve IX). This nerve synapses with the otic ganglion (a collection of neuronal cell bodies). The auriculotemporal nerve then carries parasympathetic fibres from the otic ganglion to the parotid gland. Parasympathetic stimulation causes an increase in saliva production.
Sympathetic innervation originates from the superior cervical ganglion, part of the paravertebral chain. Fibres from this ganglion travel along the external carotid artery to reach the parotid gland. Increased activity of the sympathetic nervous system inhibits saliva secretion, via vasoconstriction.
Clinical Relevance: Disorders of the Parotid Gland
Parotid Gland Tumours
The parotid gland is the most common site of a salivary gland tumour. These tumours are usually benign, such as an adenolymphoma. In contrast, tumours of the submandibular and sublingual glands are less common, but more likely to be malignant.
Treatment usually involves surgical excision of the tumour and parotid gland, known as a parotidectomy. During this procedure, it is critical to identify and preserve the facial nerve and its branches.
Damage to facial nerve or its branches will cause paralysis of the facial muscles. The affected muscles will lose tone, and the area will ‘sag’. The inferior eyelid can be particularly affected, falling away from the eyeball (known as ectropion).
Parotitis
Parotitis refers to inflammation of the parotid gland, usually as a result of an infection. The parotid gland is enclosed in a tough fibrous capsule. This restricts swelling of the gland, producing pain.
The pain produced can be referred to the external ear. This is because the auriculotemporal nerve provides sensory innervation to the parotid gland and the external ear.