The trigeminal nerve, CN V, is the fifth paired cranial nerve. It is also the largest cranial nerve. In this article, we shall look at the anatomical course of the nerve, and the motor, sensory and parasympathetic functions of its terminal branches.
The trigeminal nerve is associated with derivatives of the 1st pharyngeal arch.
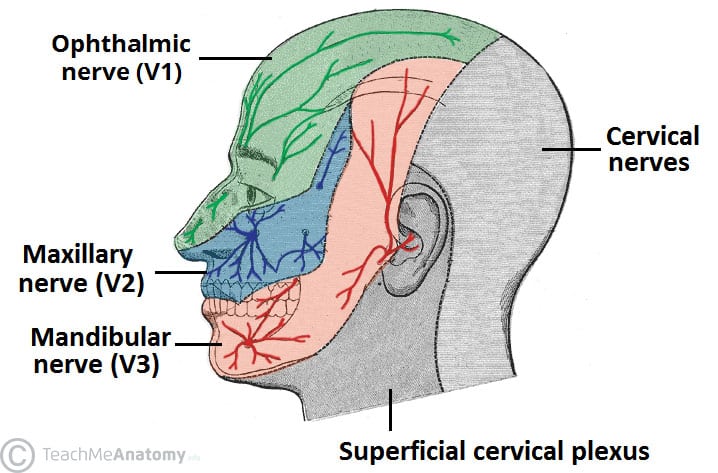
Sensory: The three terminal branches of CN V innervate the skin, mucous membranes and sinuses of the face. Their distribution pattern is similar to the dermatome supply of spinal nerves (except there is little overlap in the supply of the divisions).
Motor: Only the mandibular branch of CN V has motor fibres. It innervates the muscles of mastication: medial pterygoid, lateral pterygoid, masseter and temporalis. The mandibular nerve also supplies other 1st pharyngeal arch derivatives: anterior belly of digastric, mylohyoid, tensor veli palatini and tensor tympani.
Parasympathetic Supply: The post-ganglionic neurones of parasympathetic ganglia travel with branches of the trigeminal nerve. (But note that CN V is NOT part of the cranial outflow of PNS supply)
Anatomical Course
The trigeminal nerve originates from three sensory nuclei (mesencephalic, principal sensory, spinal nuclei of trigeminal nerve) and one motor nucleus (motor nucleus of the trigeminal nerve) extending from the midbrain to the medulla. A nucleus (pl. nuclei) is a collection of neurone cell bodies within the central nervous system.
At the level of the pons, the sensory nuclei merge to form a sensory root. The motor nucleus continues to form a motor root. These roots are analogous to the dorsal and ventral roots of the spinal cord.
In the middle cranial fossa, the sensory root expands into the trigeminal ganglion. A ganglion (pl. ganglia) refers to a collection of the neurone cell bodies outside the central nervous system. The trigeminal ganglion is located lateral to the cavernous sinus, in a depression of the temporal bone. This depression is known as the trigeminal cave.
The peripheral aspect of the trigeminal ganglion gives rise to 3 divisions: ophthalmic (V1), maxillary (V2) and mandibular (V3).
The motor root passes inferiorly to the sensory root, along the floor of the trigeminal cave. Its fibres are only distributed to the mandibular division.
The ophthalmic nerve and maxillary nerve travel lateral to the cavernous sinus exiting the cranium via the superior orbital fissure and foramen rotundum respectively. The mandibular nerve exits via the foramen ovale entering the infra-temporal fossa. (Note – be aware that while we talk about the nerves exiting the cranial cavity, the sensory components can also be said to be entering the cranial cavity, since they are afferent fibres).
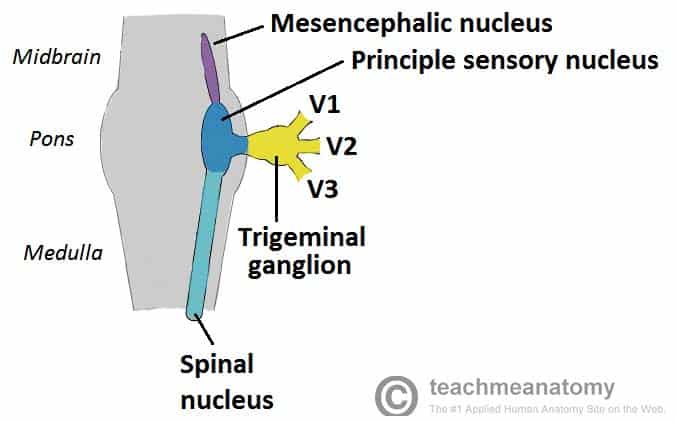
Fig 1 – The origin of the sensory aspect of the trigeminal nerve. Note that the nuclei are situated within in the CNS, and the ganglia outside the CNS.
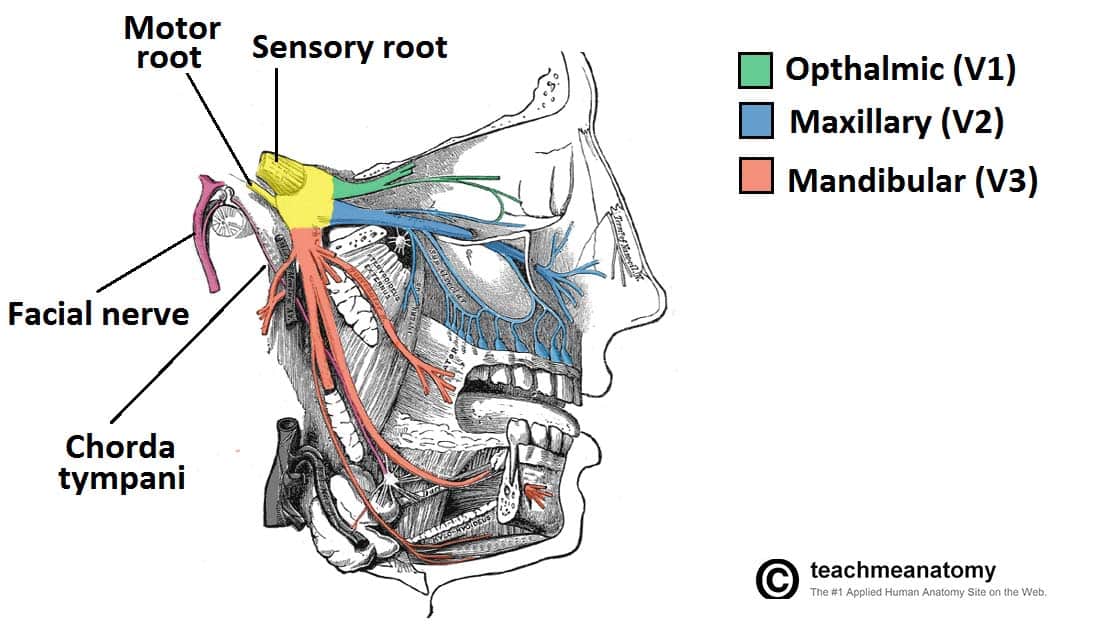
Fig 2 – Overview of the deep distribution of the trigeminal nerve and its terminal branches.
Divisions
Ophthalmic Nerve
Ophthalmic nerve gives rise to 3 terminal branches: frontal, lacrimal and nasociliary, which innervate the skin and mucous membrane of derivatives of the frontonasal prominence derivatives:
- Forehead and scalp
- Frontal and ethmoidal sinus
- Upper eyelid and its conjunctiva
- Cornea (see clinical relevance)
- Dorsum of the nose
Parasympathetic Supply:
- Lacrimal gland: Post ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve), travel with the zygomatic branch of V2 and then join the lacrimal branch of V1. The fibres supply parasympathetic innervation to the lacrimal gland.
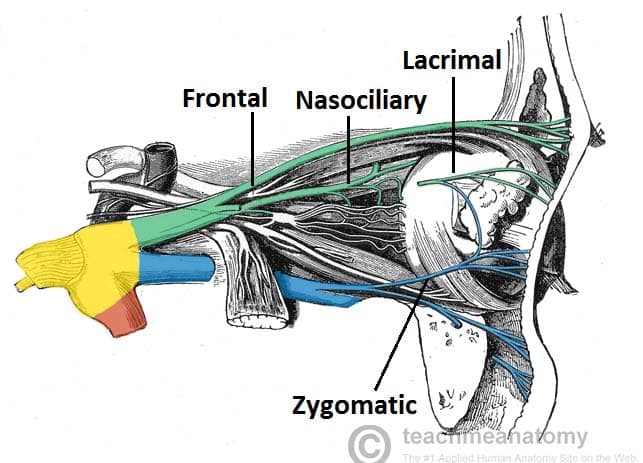
Fig 3 – Nervous supply to the orbit from the ophthalmic and maxillary nerves. (other nerves e.g. orbital, not labelled). Note that the lacrimal nerve has been partly removed to expose the underlying structures.
Clinical Relevance: Corneal Reflex
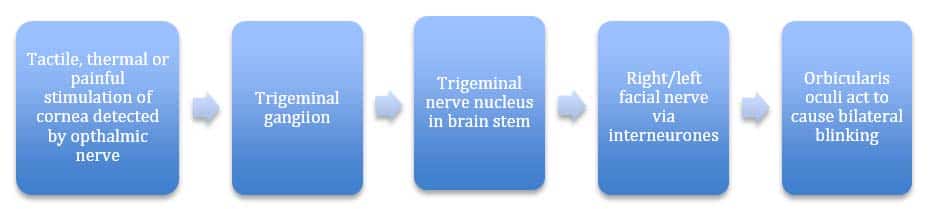
The corneal reflex is the involuntary blinking of the eyelids – stimulated by tactile, thermal or painful stimulation of the cornea.
In the corneal reflex, the ophthalmic nerve acts as the afferent limb – detecting the stimuli. The facial nerve is the efferent limb, causing contraction of the orbicularis oculi muscle.
If the corneal reflex is absent, it is a sign of damage to the trigeminal/ophthalmic nerve, or the facial nerve.
Maxillary Nerve
Maxillary nerve gives rise to 14 terminal branches, which innervate the skin, mucous membranes and sinuses of derivatives of the maxillary prominence of the 1st pharyngeal arch:
- Lower eyelid and its conjunctiva
- Cheeks and maxillary sinus
- Nasal cavity and lateral nose
- Upper lip
- Upper molar, incisor and canine teeth and the associated gingiva
- Superior palate
Parasympathetic Supply:
- Lacrimal gland: Post ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve), travel with the zygomatic branch of V2 and then join the lacrimal branch of V1. The fibres supply parasympathetic innervation to the lacrimal gland.
- Nasal glands: Parasympathetic fibres are also carried to the mucous glands of the nasal mucosa. Post-ganglionic fibres travel with the nasopalatine and greater palatine nerves (branches of V2)
Mandibular Nerve
Mandibular nerve gives rise to four terminal branches in the infra-temporal fossa: buccal nerve, inferior alveolar nerve, auriculotemporal nerve and lingual nerve.
These branches innervate the skin, mucous membrane and striated muscle derivatives of the mandibular prominence of the 1st pharyngeal arch.
Sensory supply:
- Mucous membranes and floor of the oral cavity
- External ear
- Lower lip
- Chin
- Anterior 2/3 of the tongue (only general sensation; special taste sensation supplied by the chorda tympani, a branch of the facial nerve)
- Lower molar, incisor and canine teeth and the associated gingiva
Motor Supply:
- Muscles of mastication; medial pterygoid, lateral pterygoid, masseter, temporalis
- Anterior belly of the digastric muscle and the mylohyoid muscle (these are suprahyoid muscles)
- Tensor veli palatini
- Tensor tympani
Parasympathetic Supply:
- Submandibular and Sublingual glands: Post-ganglionic fibres from the submandibular ganglion (derived from the facial nerve), travel with the lingual nerve to innervate these glands.
- Parotid gland: Post-ganglionic fibres from the otic ganglion (derived from the glossopharyngeal nerve, CN IX), travel with the auriculotemporal branch of the V3 to innervate the parotid gland.
Clinical Relevance: Inferior Alveolar Nerve Block
The inferior alveolar nerve, a branch of V3, travels through the mandibular foramen and mandibular canal. Within the mandibular canal, the inferior alveolar nerve forms the inferior dental plexus, which innervates the lower teeth. A major branch of this plexus, the mental nerve, supplies the skin and mucous membranes of the lower lip, skin of the chin, and the gingiva of the lower teeth.
In some dental procedures which require a local anaesthesia, the inferior alveolar nerve is blocked before it gives rise to the plexus.
The anaesthetic solution is administered at the mandibular foramen, causing numbness of area supplied by the inferior alveolar nerve. The anaesthetic fluid also spreads to the lingual nerve which originates near the inferior alveolar nerve, causing numbness of the anterior 2/3 of the tongue.
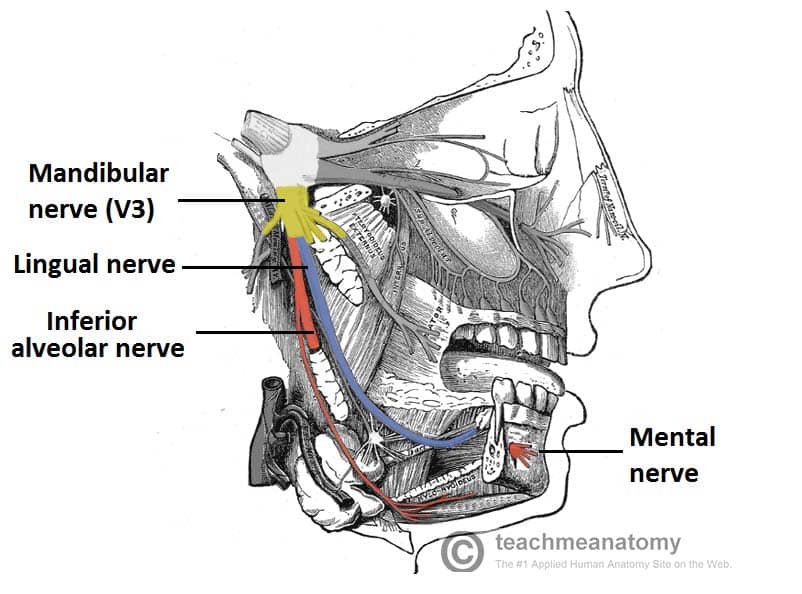
Fig 6 – Anatomical course of the inferior alveolar and lingual nerves. Note the close proximity of the two nerves. The portion of the inferior alveolar nerve that runs through the mandibular canal has been removed.
Clinical Relevance: Examination of the Trigeminal Nerve
- Testing sensory supply: ask the patient to close their eyes and introduce a cotton wisp to areas of the face supplied by the three divisions of the trigeminal nerve to detect tactile sensory competence.
- Testing motor supply: ask the patient to clench their jaw as you palpate superior to the zygomatic arch to feel for contraction of the temporalis and then repeat palpating inferiorly for the masseter. Ask the patient to open their mouth and deviate their mandible to the right and left to check for competence of the medial and lateral pterygoid muscles.
- Test for corneal reflex – note this requires a competent ophthalmic branch and temporal and zygomatic branches of the facial nerve.