The facial nerve (CN VII) is the seventh paired cranial nerve.
In this article, we shall look at the anatomy of the facial nerve – its anatomical course, functions and clinical correlations.
Overview
The facial nerve is associated with the derivatives of the second pharyngeal arch:
- Motor – muscles of facial expression, posterior belly of the digastric, stylohyoid and stapedius muscles.
- Sensory – a small area around the concha of the external ear.
- Special Sensory – provides special taste sensation to the anterior 2/3 of the tongue via the chorda tympani
- Parasympathetic – supplies many of the glands of the head and neck, including:
- Submandibular and sublingual salivary glands.
- Nasal, palatine and pharyngeal mucous glands.
- Lacrimal glands.
Anatomical Course
The course of the facial nerve is very complex. There are many branches, which transmit a combination of sensory, motor and parasympathetic fibres.
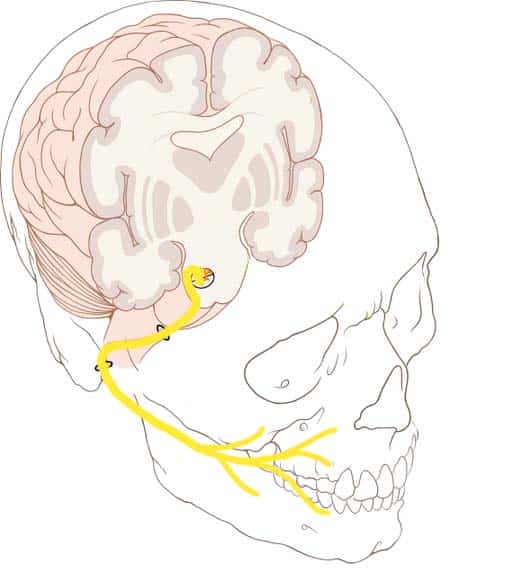
Anatomically, the course of the facial nerve can be divided into two parts:
- Intracranial – the course of the nerve through the cranial cavity, and the cranium itself.
- Extracranial – the course of the nerve outside the cranium, through the face and neck.
Intracranial
The nerve arises in the pons, an area of the brainstem. It begins as two roots; a large motor root, and a small sensory root (the part of the facial nerve that arises from the sensory root is sometimes known as the intermediate nerve).
The two roots travel through the internal acoustic meatus, a 1cm long opening in the petrous part of the temporal bone. Here, they are in very close proximity to the inner ear.
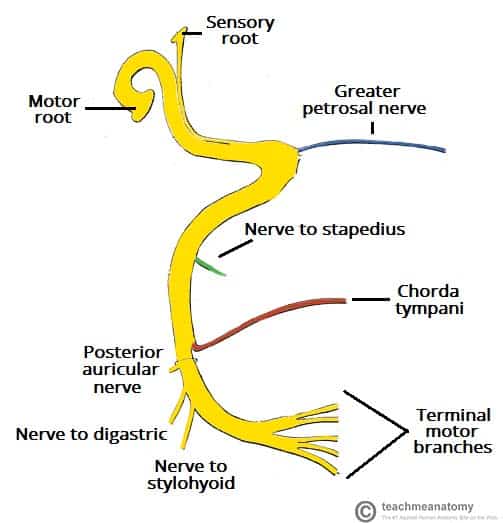
Still within the temporal bone, the roots leave the internal acoustic meatus, and enter into the facial canal. The canal is a ‘Z’ shaped structure. Within the facial canal, three important events occur:
- Firstly the two roots fuse to form the facial nerve.
- Next, the nerve forms the geniculate ganglion (a ganglion is a collection of nerve cell bodies).
- Lastly, the nerve gives rise to:
- Greater petrosal nerve – parasympathetic fibres to mucous glands and lacrimal gland.
- Nerve to stapedius – motor fibres to stapedius muscle of the middle ear.
- Chorda tympani – special sensory fibres to the anterior 2/3 tongue and parasympathetic fibres to the submandibular and sublingual glands.
The facial nerve then exits the facial canal (and the cranium) via the stylomastoid foramen. This is an exit located just posterior to the styloid process of the temporal bone.
Extracranial
After exiting the skull, the facial nerve turns superiorly to run just anterior to the outer ear.
The first extracranial branch to arise is the posterior auricular nerve. It provides motor innervation to the some of the muscles around the ear. Immediately distal to this, motor branches are sent to the posterior belly of the digastric muscle and to the stylohyoid muscle.
The main trunk of the nerve, now termed the motor root of the facial nerve, continues anteriorly and inferiorly into the parotid gland (note – the facial nerve does not contribute towards the innervation of the parotid gland, which is innervated by the glossopharyngeal nerve).
Within the parotid gland, the nerve terminates by splitting into five branches:
- Temporal branch
- Zygomatic branch
- Buccal branch
- Marginal mandibular branch
- Cervical branch
These branches are responsible for innervating the muscles of facial expression.
Motor Functions
Branches of the facial nerve are responsible for innervating many of the muscles of the head and neck. All these muscles are derivatives of the second pharyngeal arch.
The first motor branch arises within the facial canal; the nerve to stapedius. It passes through the pyramidal eminence to supply the stapedius muscle in the middle ear.
Between the stylomastoid foramen, and the parotid gland, three more motor branches are given off:
- Posterior auricular nerve – Ascends in front of the mastoid process, and innervates the intrinsic and extrinsic muscles of the outer ear. It also supplies the occipital part of the occipitofrontalis muscle.
- Nerve to the posterior belly of the digastric muscle – Innervates the posterior belly of the digastric muscle (a suprahyoid muscle of the neck). It is responsible for raising the hyoid bone.
- Nerve to the stylohyoid muscle – Innervates the stylohyoid muscle (a suprahyoid muscle of the neck). It is responsible for raising the hyoid bone.
Within the parotid gland, the facial nerve terminates by bifurcating into five motor branches. These innervate the muscles of facial expression:
- Temporal – Innervates the frontalis, orbicularis oculi and corrugator supercilii.
- Zygomatic – Innervates the orbicularis oculi.
- Buccal – Innervates the orbicularis oris, buccinator and zygomaticus.
- Marginal mandibular – Innervates the depressor labii inferioris, depressor anguli oris and mentalis.
- Cervical – Innervates the platysma.
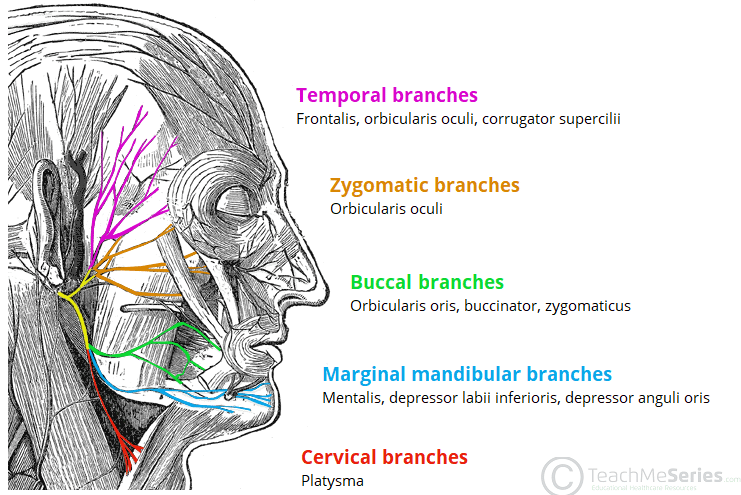
Fig 3 – Innervation to the muscles of facial expression via the facial nerve (CN VII)
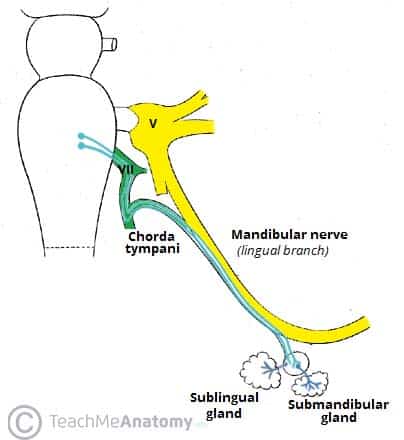
Special Sensory Functions
The chorda tympani branch of the facial nerve is responsible for innervating the anterior 2/3 of the tongue with the special sense of taste.
The nerve arises in the facial canal, and travels across the bones of the middle ear, exiting via the petrotympanic fissure, and entering the infratemporal fossa.
Within the infratemporal fossa, the chorda tympani ‘hitchhikes’ upon the lingual nerve. The parasympathetic fibres of the chorda tympani stay with the lingual nerve, but the main body of the nerve leaves to innervate the anterior 2/3 of the tongue.
Parasympathetic Functions
The parasympathetic fibres of the facial nerve are carried by the greater petrosal and chorda tympani branches.
Greater Petrosal Nerve
The greater petrosal nerve arises immediately distal to the geniculate ganglion within the facial canal. It then moves in anteromedial direction, exiting the temporal bone into the middle cranial fossa. From here, its travels across (but not through) the foramen lacerum, combining with the deep petrosal nerve to form the nerve of the pterygoid canal.
The nerve of pterygoid canal then passes through the pterygoid canal (Vidian canal) to enter the pterygopalatine fossa, and synapses with the pterygopalatine ganglion. Branches from this ganglion then go on to provide parasympathetic innervation to the mucous glands of the oral cavity, nose and pharynx, and the lacrimal gland.
Chorda Tympani
The chorda tympani also carries some parasympathetic fibres. These combine with the lingual nerve (a branch of the trigeminal nerve) in the infratemporal fossa and form the submandibular ganglion. Branches from this ganglion travel to the submandibular and sublingual salivary glands.
Clinical Relevance: Damage to the Facial Nerve
The facial nerve has a wide range of functions. Thus, damage to the nerve can produce a varied set of symptoms, depending on the site of the lesion.
Intracranial Lesions
Intracranial lesions occur during the intracranial course of the facial nerve (proximal to the stylomastoid foramen).
The muscles of facial expression will be paralysed or severely weakened. The other symptoms produced depend on the location of the lesion, and the branches that are affected:
- Chorda tympani – reduced salivation and loss of taste on the ipsilateral 2/3 of the tongue.
- Nerve to stapedius – ipsilateral hyperacusis (hypersensitive to sound).
- Greater petrosal nerve – ipsilateral reduced lacrimal fluid production.
The most common cause of an intracranial lesion of the facial nerve is infection related to the external or middle ear. If no definitive cause can be found, the disease is termed Bell’s palsy.

Fig 5 – Right sided weakness of the muscles of facial expression, due to facial nerve paralysis.
Extracranial Lesions
Extracranial lesions occur during the extracranial course of the facial nerve (distal to the stylomastoid foramen). Only the motor function of the facial nerve is affected, therefore resulting in paralysis or severe weakness of the muscles of facial expression.
There are various causes of extracranial lesions of the facial nerve:
- Parotid gland pathology – e.g a tumour, parotitis, surgery.
- Infection of the nerve – particularly by the herpes virus.
- Compression during forceps delivery – the neonatal mastoid process is not fully developed and does not provide complete protection of the nerve.
- Idiopathic – If no definitive cause can be found then the disease is termed Bell’s palsy.
Prosection Images
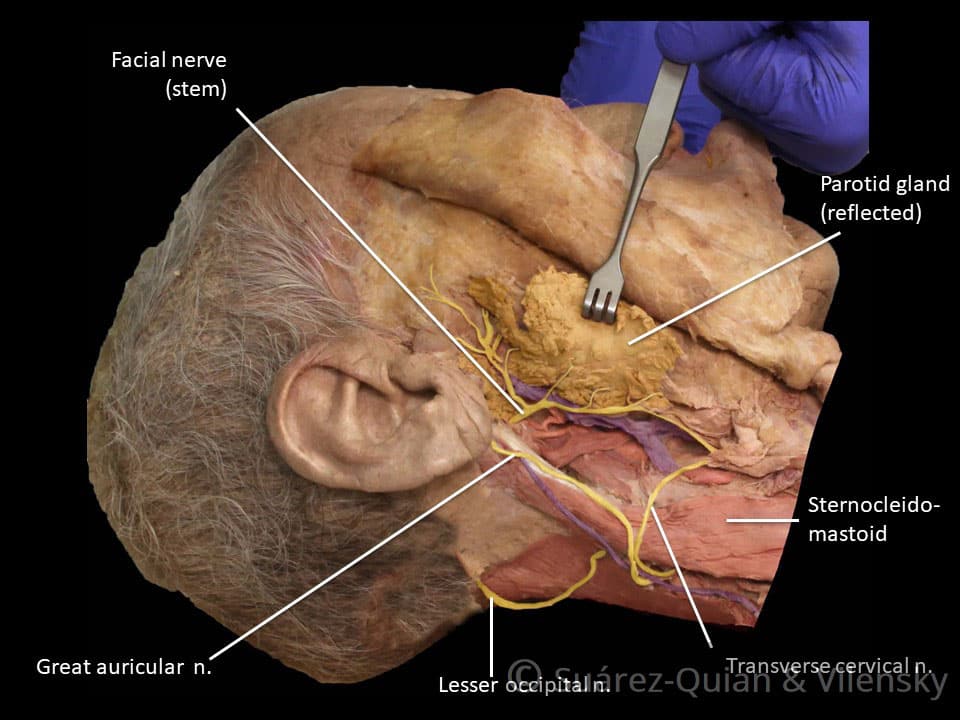
Dissection 1 – Relationship of the facial nerve and parotid gland. Image from All in One Anatomy Review.
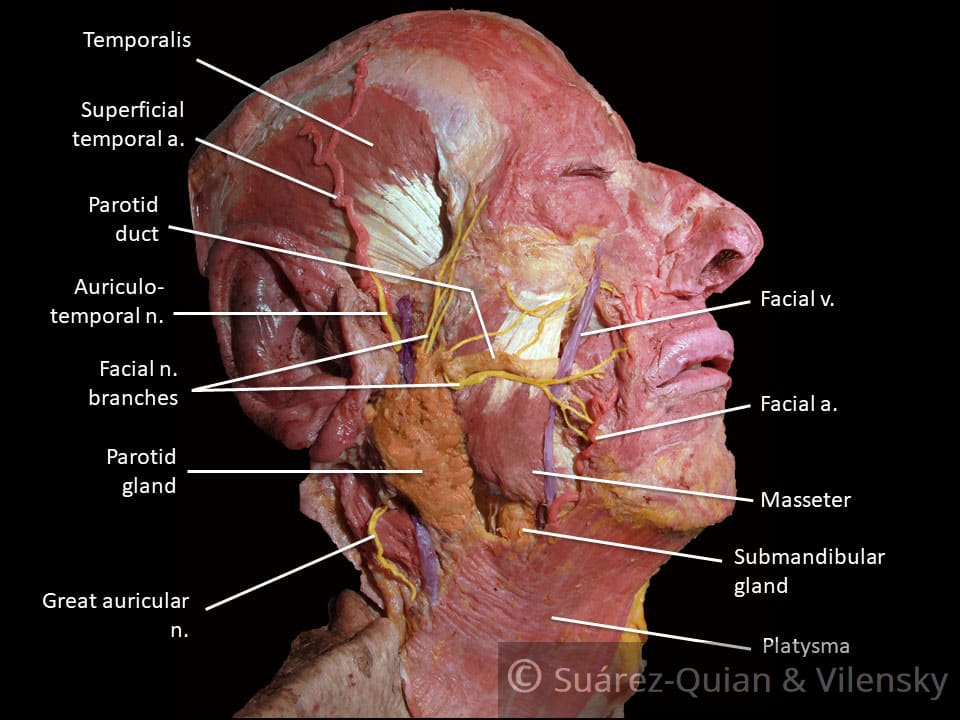
Dissection 2 – Demonstrating the branches of the facial nerve. Image from All in One Anatomy Review.