The anal canal is the final segment of the gastrointestinal tract.
It has an important role in defecation and maintaining faecal continence.
In this article, we shall look at the anatomy of the anal canal – its position, structure, relations and neurovascular supply.
Anatomical Position
The anal canal is located within the anal triangle of the perineum between the right and left ischioanal fossae. It is the final segment of the gastrointestinal tract, around 4cm in length.
The canal begins as a continuation of the rectum and passes inferoposteriorly to terminate at the anus.
Anatomical Structure
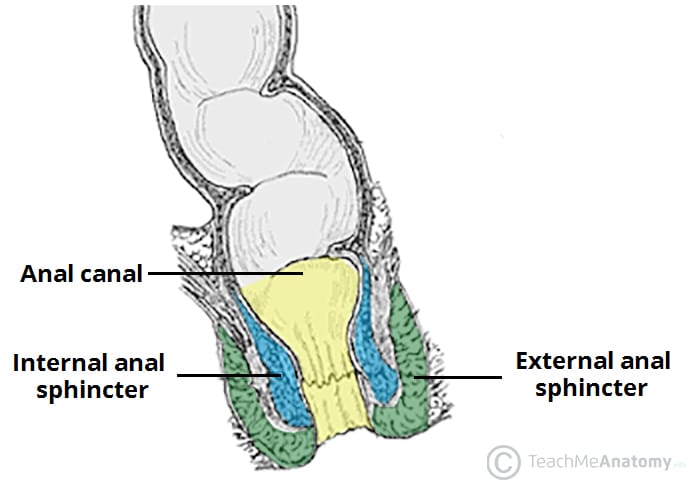
Except during defecation, the anal canal is collapsed by the internal and external anal sphincters to prevent the passage of faecal material.
Anal Sphincters
The anal canal is surrounded by internal and external anal sphincters, which play a crucial role in the maintenance of faecal continence:
- Internal anal sphincter – surrounds the upper 2/3 of the anal canal. It is formed from a thickening of the involuntary circular smooth muscle in the bowel wall.
- External anal sphincter – voluntary muscle that surrounds the lower 2/3 of the anal canal (and so overlaps with the internal sphincter). It blends superiorly with the puborectalis muscle of the pelvic floor.
At the junction of the rectum and the anal canal, there is a muscular ring – known as the anorectal ring. It is formed by the fusion of the internal anal sphincter, external anal sphincter and puborectalis muscle, and is palpable on digital rectal examination.
Internal Structure
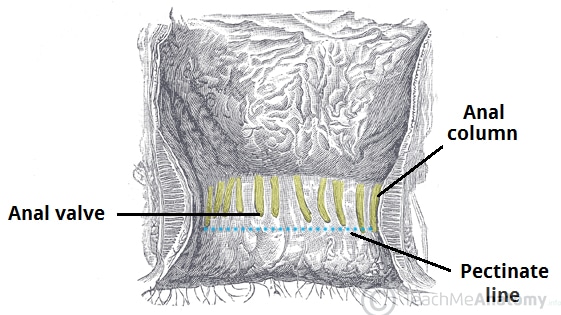
The superior aspect of the anal canal has the same epithelial lining as the rectum (columnar epithelium). However, in the anal canal, the mucosa is organised into longitudinal folds, known as anal columns. These are joined at their inferior ends by anal valves. Above the anal valves are small pouches which are referred to as anal sinuses – these contain glands that secrete mucus.
The anal valves collectively form an irregular circle – known as the pectinate line (or dentate line). This line divides the anal canal into upper and lower parts, which differ in both structure and neurovascular supply. This is a result of their different embryological origins:
- Above the pectinate line – derived from the embryonic hindgut.
- Below the pectinate line – derived from the ectoderm of the proctodeum.
Inferior to the pectinate line, the anal canal is lined by non-keratinised stratified squamous epithelium (known as the anal pecten). It is a pale and smooth surface, which transitions at the level of the intersphincteric groove to true skin (keratinised stratified squamous).
Anatomical Relations
The anal canal lies in close proximity to several other important structures in the pelvis and perineum:
| Anteriorly | Posteriorly | Laterally | |
| Male | Female |
|
|
|
|
||
Neurovascular Supply and Lymphatics
As discussed above, the pectinate line divides the anal canal into two parts – which have a different arterial supply, venous drainage, innervation and lymphatic drainage.
| Modality | Above Pectinate line | Below Pectinate line |
| Arterial Supply |
|
|
| Venous Drainage |
|
|
| Nerve Supply |
|
|
| Lymphatics |
|
|
Clinical Relevance – Haemorrhoids
Haemorrhoids are vascular cushions found within the anal canal of healthy individuals, which help with the maintenance faecal continence. If they become swollen and distended, they are referred to as pathological haemorrhoids.
Pathological haemorrhoids are observed in people who suffer from constipation, prolonged straining when defecating, or raised intra-abdominal pressure (e.g pregnancy, ascites). Upon examination of the anal canal (with the patient in the lithotomy position), the haemorrhoids are typically located at the 3, 7 and 11 o’clock positions.
They can cause bleeding and itchiness, and depending on the severity, can be managed conservatively or surgically.