The bladder is an organ of the urinary system. It plays two main roles:
- Temporary storage of urine – the bladder is a hollow organ with distensible walls. It has a folded internal lining (known as rugae), which allows it to accommodate up to 400-600ml of urine in healthy adults.
- Assists in the expulsion of urine – the musculature of the bladder contracts during micturition, with concomitant relaxation of the sphincters.
In this article, we shall look at the anatomy of the bladder – its shape, vasculature and neurological control.
Shape of the Bladder
The appearance of the bladder varies depending on the amount of urine stored. When full, it exhibits an oval shape, and when empty it is flattened by the overlying bowel.
The external features of the bladder are:
- Apex – located superiorly, pointing towards the pubic symphysis. It is connected to the umbilicus by the median umbilical ligament (a remnant of the urachus).
- Body – main part of the bladder, located between the apex and the fundus
- Fundus (or base) – located posteriorly. It is triangular-shaped, with the tip of the triangle pointing backwards.
- Neck – formed by the convergence of the fundus and the two inferolateral surfaces. It is continuous with the urethra.
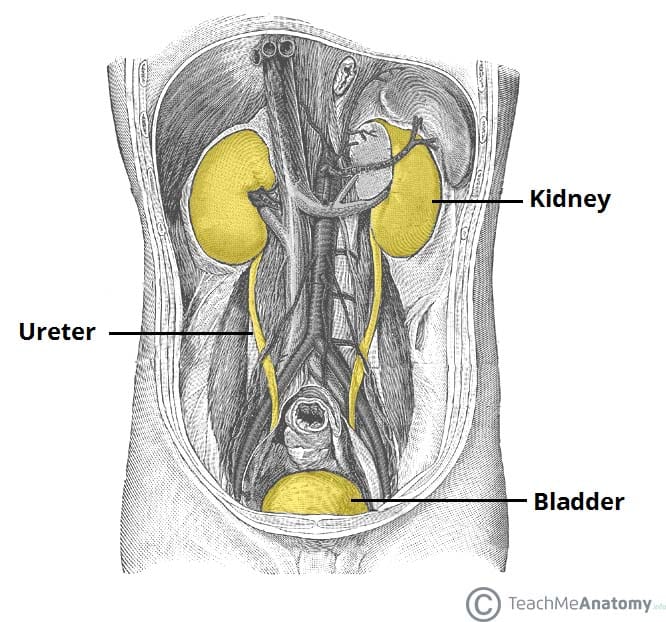
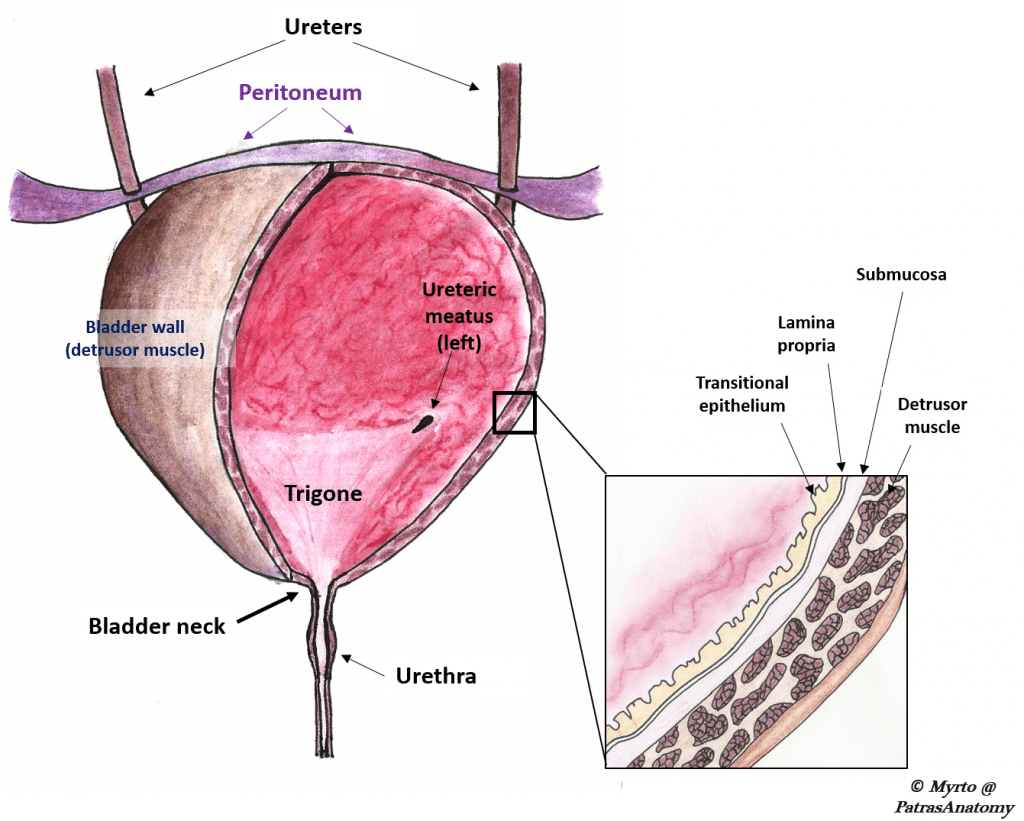
Urine enters the bladder through the left and right ureters, and exits via the urethra. Internally, these orifices are marked by the trigone – a triangular area located within the fundus.
In contrast to the rest of the internal bladder, the trigone has smooth walls (this is explained by the different embryological origin: the trigone is developed by the integration of two mesonephric ducts at the base of the bladder).
Musculature
The musculature of the bladder plays a key role in the storage and emptying of urine.
In order to contract during micturition, the bladder wall contains specialised smooth muscle – known as detrusor muscle. Its fibres are orientated in multiple directions, thus retaining structural integrity when stretched. It receives innervation from both the sympathetic and parasympathetic nervous systems.
The fibres of the detrusor muscle often become hypertrophic (presenting as prominent trabeculae) in order to compensate for increased workload of the bladder emptying. This is very common in conditions that obstruct the urine outflow such as benign prostatic hyperplasia.
There are also two muscular sphincters located in the urethra:
- Internal urethral sphincter:
- Male – consists of circular smooth fibres, which are under autonomic control. It is thought to prevent seminal regurgitation during ejaculation.
- Females – thought to be a functional sphincter (i.e. no sphincteric muscle present). It is formed by the anatomy of the bladder neck and proximal urethra.
- External urethral sphincter – has the same structure in both sexes. It is skeletal muscle, and under voluntary control. However, in males the external sphincteric mechanism is more complex, as it correlates with fibres of the rectourethralis muscle and the levator ani muscle.
Vasculature
The vasculature of the bladder is primarily derived from the internal iliac vessels.
Arterial supply is via the superior vesical branch of the internal iliac artery. In males, this is supplemented by the inferior vesical artery, and in females by the vaginal arteries. In both sexes, the obturator and inferior gluteal arteries may also contribute small branches.
Venous drainage is achieved by the vesical venous plexus, which empties into the internal iliac veins. The vesical plexus in males is in continuity at the retropubic space with the prostate venous plexus (plexus of Santorini), which also receives blood from the dorsal vein of the penis
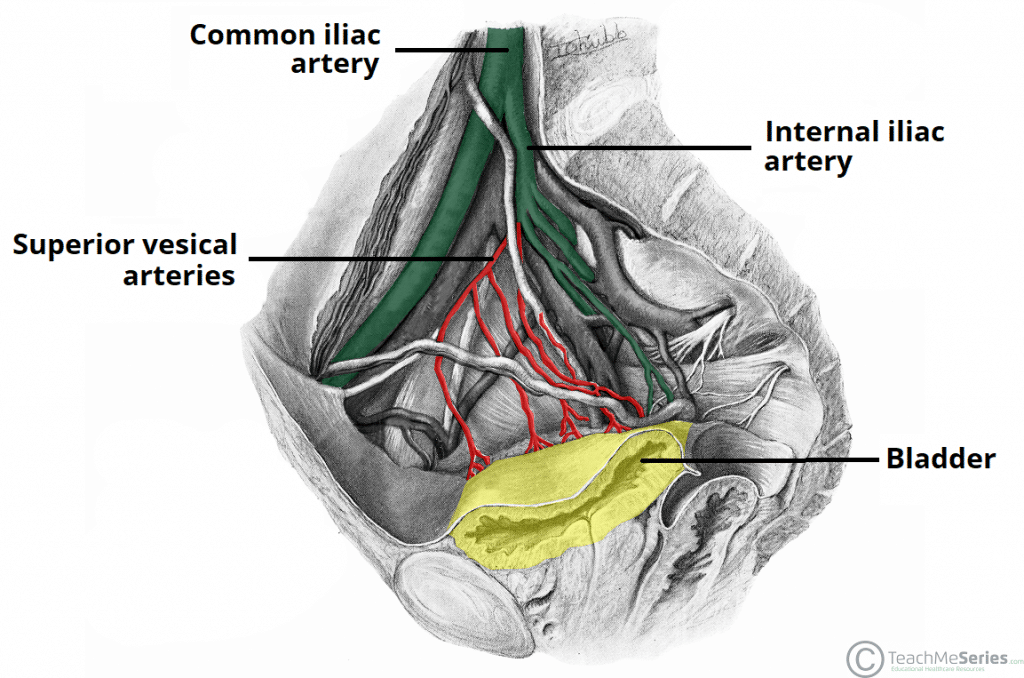
Fig 4 – Arterial supply to the bladder via the superior vesical arteries.
Lymphatics
The superolateral aspect of the bladder drains into the external iliac lymph nodes. The neck and fundus drain into the internal iliac, sacral and common iliac nodes.
Nervous Supply
Neurological control is complex, with the bladder receiving input from both the autonomic (sympathetic and parasympathetic) and somatic arms of the nervous system:
- Sympathetic – hypogastric nerve (T12 – L2). It causes relaxation of the detrusor muscle, promoting urine retention.
- Parasympathetic – pelvic nerve (S2-S4). Increased signals from this nerve causes contraction of the detrusor muscle, stimulating micturition.
- Somatic – pudendal nerve (S2-4). It innervates the external urethral sphincter, providing voluntary control over micturition.
In addition to the efferent nerves supplying the bladder, there are sensory (afferent) nerves that report to the brain. They are found in the bladder wall and signal the need to urinate when the bladder becomes full.
The Bladder Stretch Reflex
The bladder stretch reflex is a primitive spinal reflex, in which micturition is stimulated in response to stretch of the bladder wall. It is analogous to a muscle spinal reflex, such as the patella reflex.
During toilet training in infants, this spinal reflex is overridden by the higher centres of the brain, to give voluntary control over micturition.
The reflex arc:
- Bladder fills with urine, and the bladder walls stretch. Sensory nerves detect stretch and transmit this information to the spinal cord.
- Interneurons within the spinal cord relay the signal to the parasympathetic efferents (the pelvic nerve).
- The pelvic nerve acts to contract the detrusor muscle, and stimulate micturition.
Although it is non-functional post childhood, the bladder stretch reflex needs to be considered in spinal injuries (where the descending inhibition cannot reach the bladder), and in neurodegenerative diseases (where the brain is unable to generate inhibition).
Clinical Relevance: Spinal Cord Injuries and the Bladder
The bladder has important clinical considerations when it comes to spinal cord lesions. There are two different clinical syndromes, depending on where the damage has occurred.
Reflex Bladder – Spinal Cord Transection Above T12
In this case, the afferent signals from the bladder wall are unable to reach the brain, and the patient will have no awareness of bladder filling. There is also no descending control over the external urethral sphincter, and it is constantly relaxed.
There is a functioning spinal reflex, where the parasympathetic system initiates detrusor contraction in response to bladder wall stretch. Thus, the bladder automatically empties as it fills – known as the reflex bladder.
Flaccid Bladder – Spinal Cord Transection Below T12
A spinal cord transection at this level will have damaged the parasympathetic outflow to the bladder. The detrusor muscle will be paralysed, unable to contract. The spinal reflex does not function.
In this scenario, the bladder will fill uncontrollably, becoming abnormally distended until overflow incontinence occurs.
Clinical Relevance: Urine Retention
Besides neurogenic dysfunction of the bladder, normal bladder emptying may be hampered by any form of obstruction, from the level of the bladder neck downwards. In males, the most common cause is obstruction due to prostate enlargement (BPH). Other causes include obstruction by a stone or large blood clot.
Acute retention is a medical emergency, as the bladder has a “normal” functional capacity with is pushed to the limit due to accumulation of urine in an acutely obstructed reservoir. The patient feels increasingly excruciating pain and the placement of a urinary catheter alleviates the symptoms immediately.
Chronic retention is a gradual procedure due to incomplete obstruction of the urine outflow. This leads to accumulation of residual urine in the bladder through months or even years; the bladder is therefore progressively distended in volumes that exceed 1-1.5 lt of urine.
Chronic retention is often accompanied by impairment of renal function. However no pain is usually present as the bladder is gradually stretched. Chronic retention of urine is often complicated by infections and formation of bladder stones due to urine stasis and accumulation of minerals in the urine